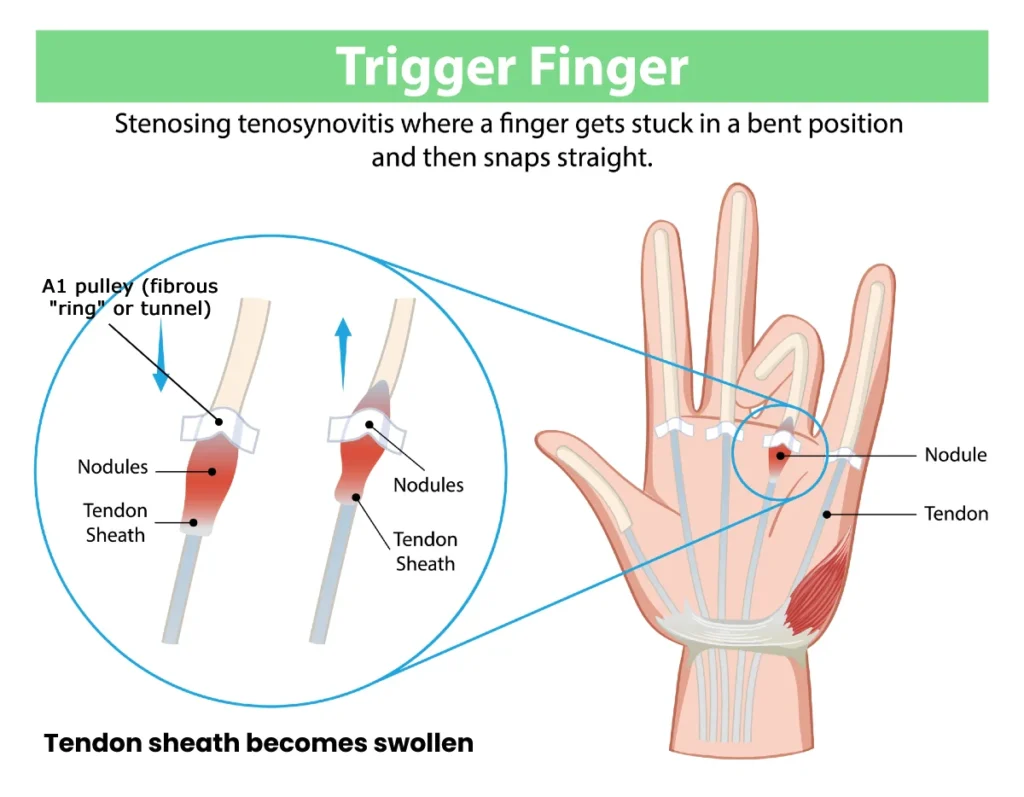
Trigger finger, medically known as stenosing tenosynovitis, is a condition in which the flexor tendon of a finger catches or becomes stuck while passing through its narrow tunnel (pulley). This makes finger bending and straightening difficult and often causing a characteristic “snapping” or clicking sensation. It develops as a result of inflammation and thickening of the tendon and its sheath, or of the pulley mechanism, which disrupts smooth tendon gliding and leads to pain, stiffness, or a catching sensation during movement.
In the early stages, symptoms may be mild and limited to slight discomfort or morning stiffness. Over time, however, they can worsen, and the finger may occasionally become locked in a bent position. Stenosing tenosynovitis can affect any finger and is more common in people who perform repetitive hand movements, have certain medical conditions, or are exposed to prolonged hand strain.
In this article, we explain what is trigger finger, discuss its causes and how to recognize its symptoms, outline available treatment options including exercises, and describe what you can do to relieve symptoms and prevent the condition from worsening.
What Is Trigger Finger?
Definition:
Trigger finger, medically known as stenosing tenosynovitis, is a condition in which the flexor tendon of the finger has difficulty gliding smoothly through its sheath. As a result, the finger may “catch,” lock, or suddenly snap when bending or straightening.
This occurs due to inflammation and thickening of the tendon, its surrounding sheath, or the wall of the fibrous tunnel through which the tendon passes. The main symptoms include pain, stiffness, a sensation of catching or locking in the finger, and difficulty fully extending the finger—especially in the morning.
Trigger Finger Anatomy
Normal finger flexion is enabled by the flexor tendons, which run along the palmar side of the fingers and transmit force from the forearm muscles to the phalanges. During movement, these tendons must glide smoothly back and forth to allow effortless bending and straightening of the fingers.
The tendons are surrounded by a tendon sheath, a thin tubular structure containing a small amount of lubricating synovial fluid. This sheath reduces friction and facilitates smooth tendon motion during finger movements.
Along each finger, the flexor tendons pass through a system of fibrous pulleys (A1–A5 pulleys). These pulley structures are strong connective tissue bands that hold the tendons close to the bone, preventing bowstringing and ensuring efficient force transmission.
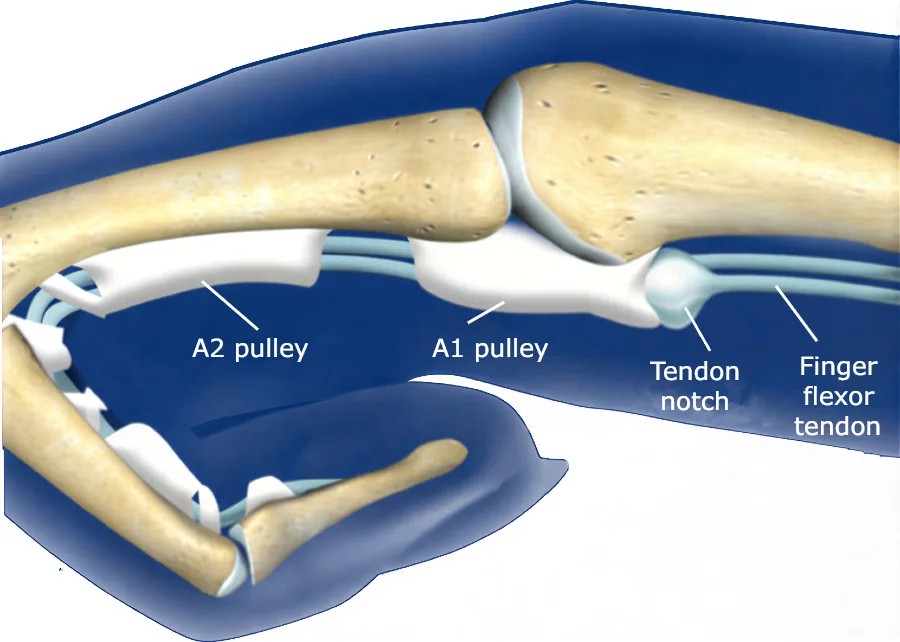
The A1 pulley, located at the level of the metacarpophalangeal (MCP) joint, plays a key anatomical role in stenosing tenosynovitis, as it is the most common site where abnormal tendon–pulley interaction occurs.
In healthy conditions, the coordinated function of the flexor tendons, tendon sheath, and pulley system allows pain-free, smooth finger motion. Disruption of this delicate anatomical relationship forms the structural basis for the development of trigger finger.
What causes trigger finger?
Trigger finger develops as a result of impaired gliding of the flexor tendon within its sheath, most often due to a combination of mechanical stress and inflammatory changes. Rather than having a single cause, it usually arises from an interaction between overuse, local tissue changes, and systemic risk factors.
Overuse and repetitive hand activities
Repetitive gripping, forceful grasping, or prolonged manual activities place increased mechanical load on the flexor tendons. Over time, this can lead to microtrauma, tendon thickening, and irritation of the tendon sheath, especially at the level of the A1 pulley.
Inflammation and tendon thickening
Chronic irritation may cause inflammation of the tendon sheath (tenosynovitis) or degenerative changes within the tendon itself. This results in narrowing of the pulley tunnel, making tendon movement less smooth and leading to catching or locking during finger motion.
Metabolic and systemic conditions
Stenosing tenosynovitis occurs more frequently in individuals with:
- Diabetes mellitus
- Rheumatoid arthritis
- Other inflammatory or metabolic disorders
In these patients, structural changes of the tendon and sheath are more common, and the condition may be more resistant to conservative treatment.
Idiopathic mechanism
In many cases, no clear cause can be identified. Even without obvious overuse or systemic disease, localized tendon degeneration or pulley thickening can develop spontaneously, particularly in middle-aged and older adults.
In summary, trigger finger is best understood as a condition caused by mechanical overload and/or inflammatory or degenerative changes that disrupt the normal interaction between the flexor tendon and the pulley system, ultimately leading to painful snapping or locking of the finger.
Stenosing Tenosynovitis Epidemiology
Stenosing tenosynovitis can affect anyone, but it is significantly more common in certain groups due to hormonal, metabolic, and mechanical factors.
It most often occurs in middle-aged and older adults, particularly between 40 and 60 years of age. Women are affected more frequently than men, likely due to hormonal influences and a higher prevalence of connective tissue disorders.
People with diabetes are at particularly high risk, with trigger finger occurring about 15% more frequently than in the general population. In diabetic patients, multiple fingers are often affected simultaneously, and symptoms tend to be more severe and prolonged. Other chronic conditions, such as rheumatoid arthritis, thyroid disorders, and systemic inflammatory diseases, also increase the likelihood of developing stenosing tenosynovitis.
Occupational or repetitive hand use is another key factor. Individuals performing repeated gripping or manual tasks—such as industrial workers, farmers, construction workers, musicians, athletes, and others using their hands extensively—are at higher risk. In fact, about 70% of cases occur in the dominant hand.
Trigger finger can also appear in children, usually as a congenital trigger thumb, which differs in cause and course from adult cases.
In summary, trigger finger is most commonly seen in middle-aged women, people with diabetes, those with chronic inflammatory conditions, and individuals who repeatedly stress their hands.
Symptoms of Stenosing Tenosynovitis
Trigger finger (stenosing tenosynovitis) typically presents as pain and unusual discomfort in the palm when moving the affected finger. A characteristic clicking or snapping sound often occurs during flexion and extension, becoming more noticeable as the condition progresses. Extending the finger is usually more difficult than bending it, as the flexor muscles and tendons are significantly stronger.
Symptoms usually start with pain at the A1 pulley area (the joint at the base of the finger near the palm). They may appear without a clear cause or after repetitive manual activity. Initially, discomfort is often worse in the morning, accompanied by stiffness. Pain can persist for months without affecting movement or progress to a complete blockage of the finger, often in the morning and eventually throughout the day. Unlocking the finger sometimes requires external assistance, such as using the other hand. In some cases, the snapping phenomenon occurs suddenly, without prior pain, and may affect one or multiple fingers simultaneously.
Although most commonly seen in the ring finger and thumb, trigger finger can affect any finger. In severe cases, the finger may remain permanently flexed, unable to actively or passively extend, or permanently extended, unable to flex.
Common Symptoms of Trigger Finger
- Pain in the palm – occurs when moving the affected finger, often near the A1 pulley area.
- Clicking or snapping sound – happens during bending and straightening of the finger.
- Temporary or persistent finger locking – most noticeable in the morning, sometimes throughout the day.
- Finger stuck in flexed or extended position – in severe cases, active movement is impossible, and unlocking may require external assistance.
Diagnosis
The diagnosis of trigger finger is primarily clinical, based on patient history and physical examination. It is suspected in individuals whose finger locks during flexion, clicks painfully, or catches when extending. The presence of a tender nodule at the base of the affected finger—usually near the junction with the palm—further supports the diagnosis.
Ultrasound is the preferred imaging method for evaluating stenosing tenosynovitis. It allows both static and dynamic assessment of the tendon, meaning the condition can be observed at rest and during finger movement. Ultrasound often reveals thickening of the pulley, as well as inflammation or irregularities of the flexor tendon.
Trigger Finger Treatment
Trigger finger can be managed in two ways—either conservatively (trigger finger treatment without surgery), which includes physical therapy, splinting, and corticosteroid injections, or surgically, by releasing the tendon when necessary. For most patients, the first-line treatment is the conservative approach, especially in mild cases or when symptoms have appeared recently.
Treatment options for trigger finger include the following:
1. Trigger Finger Exercises
In mild cases of trigger finger, especially in the early stages of the condition, exercises alone can significantly reduce symptoms and may sometimes be sufficient to improve finger function. The basic principles of rehabilitation include active tendon gliding exercises and passive stretching of the flexor tendons and joint capsules.
The main goals of these exercises are to reduce stiffness, improve smooth tendon movement within the tendon sheath, and maintain or restore mobility of the affected finger.
Recommended trigger finger exercises:
| Exercise Name | Exercise Description | Duration / Repetitions | Frequency |
|---|---|---|---|
| Hook Exercise | The fingers are actively bent at the middle and end joints while the palm remains flat, forming a shape similar to a hook or claw. This exercise promotes smooth gliding of the flexor tendons through the tendon sheath. | 20 repetitions | 2–3 times per day |
| Wrist Flexor Stretch | Using the opposite hand, the palm is gently stretched backward with the fingers fully extended, stretching the flexor tendons. | Hold for 30 seconds 2–3 repetitions |
2–3 times per day |
| Place and Hold | The finger is passively bent using the other hand and then actively held in that position without assistance. The finger is then fully straightened with the help of the other hand. | Hold for 10 seconds 10 repetitions |
2–3 times per day |
These targeted trigger finger exercises represent a useful therapeutic tool, primarily for preserving the function of the affected finger and reducing the risk of symptom recurrence.
Although in more severe cases they are often not sufficient as a standalone treatment, regular performance of these exercises plays an important role in the overall management of trigger finger.
2. Trigger Finger Splint or Brace
Splinting aims to limit flexor tendon movement and thereby reduce inflammation in the area of the affected fibrous pulley. Most commonly, a trigger finger splint or trigger finger brace is used to block the metacarpophalangeal (MCP) joint in slight flexion (about 10°–15°) or in a neutral position. The recommended duration of trigger finger splint use is typically 6 to 10 weeks.
The effectiveness of splinting is significantly lower in patients with more severe or long-standing symptoms. Although a trigger finger brace can be helpful in selected cases, in clinical practice I rarely use splints for treating trigger finger. The main reason is poor patient tolerance—splints usually need to be worn almost continuously, 24 hours a day for 6–8 weeks, which many patients find uncomfortable and restrictive in daily activities, ultimately reducing treatment compliance.
3. Extracorporeal Shock Wave Therapy (ESWT)
Extracorporeal shock wave therapy (ESWT) is widely used in the treatment of various tendinopathies, such as calcific shoulder tendinopathy, lateral epicondylitis (tennis elbow), plantar fasciitis, and others. Although the exact mechanism of action is not yet fully understood, acoustic shock waves are known to stimulate tissue healing processes, promote neovascularization in soft tissues, facilitate resorption of calcific deposits, and modulate pain through their effects on local nociceptors.
In patients with trigger finger, ESWT appears to be more effective when ultrasound findings indicate tendinosis, meaning thickening and degenerative changes of the flexor tendons, rather than pronounced inflammation and hypertrophy of the tendon sheath (tenosynovitis).
For this reason, a prior ultrasound examination is essential, as it allows precise targeting of the shock waves to the affected segment of the flexor tendon, which is most commonly located at the base of the finger, near the transition between the palm and the finger. ESWT is typically performed once weekly, for a total of 3 to 5 treatment sessions.
4. Corticosteroid Injection (Trigger Finger Injection)
Corticosteroid injection is the most commonly used and highly effective treatment for patients with trigger finger. In a trigger finger injection, the medication is injected into the flexor tendon sheath, ideally just beneath the A1 pulley, the narrow fibrous tunnel through which the tendon passes.
Corticosteroids have a strong anti-inflammatory effect. They reduce swelling of the flexor tendon, thickening of the A1 pulley, and inflammation of the tendon sheath, thereby allowing the flexor tendons to glide smoothly and freely again.
It is strongly recommended that a trigger finger injection be performed under ultrasound guidance, as this ensures accurate placement of the medication within the tendon sheath. Ultrasound-guided injection increases treatment effectiveness while significantly reducing the risk of side effects, such as subcutaneous fat atrophy or skin discoloration, which may occur if the medication leaks into surrounding tissues.
In most patients, a single targeted trigger finger injection results in significant improvement or complete resolution of symptoms within approximately 7 days. The therapeutic effect is usually long-lasting. In a smaller proportion of cases, symptoms may recur over time, in which case an additional injection may be required. Long-term studies show that even 10 years after a single corticosteroid injection, approximately 50% of patients remain completely symptom-free 1.
5. Surgical Treatment of Trigger Finger
A relatively small percentage of patients continue to experience symptoms despite appropriate conservative management. In such cases, trigger finger surgery is recommended.
Surgical treatment is considered in the following situations:
- Lack of improvement after 2–3 corticosteroid injections
- An irreducibly locked finger that cannot be actively or passively extended
Trigger finger surgery, also known as trigger finger release, is typically a straightforward procedure. It involves a small incision over the A1 pulley, after which the surgeon carefully releases the thickened fibrous band to allow the flexor tendon to glide freely again.
This procedure is highly successful and, in the vast majority of cases, results in permanent resolution of symptoms. Recurrence is relatively uncommon but is more frequently observed in patients with diabetes or in individuals who perform repetitive or heavy manual work.
Following trigger finger release, physical therapy and targeted hand exercises are important to restore full range of motion, improve strength, and achieve optimal functional recovery of the affected finger.
Conclusion on the Treatment os Stenosing Tenosynovitis
The treatment of trigger finger should be individualized and tailored to the severity of symptoms and the patient’s functional needs. In patients with mild symptoms, avoiding strenuous and repetitive manual activities combined with regular, targeted exercises may lead to significant improvement or even complete resolution of symptoms.
However, in everyday clinical practice, for the majority of patients the most effective treatment option is a corticosteroid injection under ultrasound guidance, which allows precise application and often results in rapid and substantial symptom relief. If symptom regression is incomplete, the injection can be safely repeated after 3 to 4 weeks.
When symptoms persist or recur despite 2 to 3 properly administered injections, surgical treatment should be considered. Surgery provides a definitive solution in most cases and is associated with a high success rate and full restoration of finger function.
Frequently Asked Questions (FAQ)
1. Will trigger finger go away by itself?
Mild cases of trigger finger may improve over time with rest, activity modification, and finger exercises. However, many cases do not resolve without treatment, and symptoms can persist or worsen if left unaddressed.
2. What happens if a trigger finger is not treated?
Untreated stenosing tenosynovitis can lead to increased stiffness, persistent pain, and locking of the affected finger. Over time, the finger may become permanently bent or difficult to move, making daily tasks challenging.
3. What causes trigger finger in adults?
Trigger finger in adults is usually caused by inflammation and thickening of the flexor tendon or its sheath. Risk factors include repetitive hand movements, certain medical conditions such as diabetes or rheumatoid arthritis, and long-term mechanical stress on the fingers.
4. Trigger finger treatment without surgery – is it possible?
Yes, non-surgical treatments can be effective, especially for mild to moderate cases. Options include finger exercises (tendon gliding), splints or braces to limit movement, corticosteroid injections, and extracorporeal shock wave therapy (ESWT).
5. How long does it take for a trigger finger injection to work?
Corticosteroid injections typically provide relief within a few days to a week. Most patients experience significant improvement, and the effect can be long-lasting. In some cases, a second injection may be required.
6. When surgery is necessary?
Surgery is considered when conservative treatments fail or the finger remains locked despite 2–3 properly administered injections. The procedure involves releasing the A1 pulley to allow the tendon to glide freely. Surgical outcomes are highly successful with minimal recurrence.
7. Can trigger finger affect multiple fingers?
Yes, multiple fingers can be affected, particularly in people with diabetes or chronic inflammatory conditions. However, it most commonly occurs in a single finger, often the thumb or ring finger.
8. Can lifestyle changes prevent trigger finger?
Limiting repetitive hand motions, taking breaks during prolonged manual work, and performing targeted finger exercises may help reduce the risk of developing stenosing tenosynovitis or prevent symptom progression.
Jeanmonod R, Tiwari V, Waseem M. Trigger Finger . In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Updated 2024 Feb 5.
Belloti JC, Sato ES, Faloppa F. Trigger Finger Treatment . Rev Bras Ortop (Sao Paulo). 2020;57(6):911–916. doi: 10.1055/s-0040-1713765.
Donati D, Ricci V, Boccolari P, et al. From diagnosis to rehabilitation of trigger finger: a narrative review . BMC Musculoskelet Disord. 2024;25(1):1061. doi: 10.1186/s12891-024-08192-5.
Castellanos J, Muñoz-Mahamud E, Domínguez E, et al. Long-term effectiveness of corticosteroid injections for trigger finger and thumb . J Hand Surg Am. 2015;40(1):121–126. doi: 10.1016/j.jhsa.2014.09.006.
Wojahn RD, Foeger NC, Gelberman RH, Calfee RP. Long-term outcomes following a single corticosteroid injection for trigger finger . J Bone Joint Surg Am. 2014;96(22):1849–1854. doi: 10.2106/JBJS.N.00004.