Sciatica is a condition that causes pain radiating from the lower back or buttock down the leg, most often below the knee to the foot and toes. It most commonly occurs when a herniated disc irritates or compresses nerve roots in the lumbar spine that form the sciatic nerve. In addition to pain, people may experience tingling, numbness, or muscle weakness, which can significantly interfere with daily activities.
In this article, we answer 16 essential questions about sciatica — from symptoms, duration and treatment options to when MRI or surgery may be necessary — explained clearly and based on current medical guidelines and clinical experience.
1. What is sciatica?
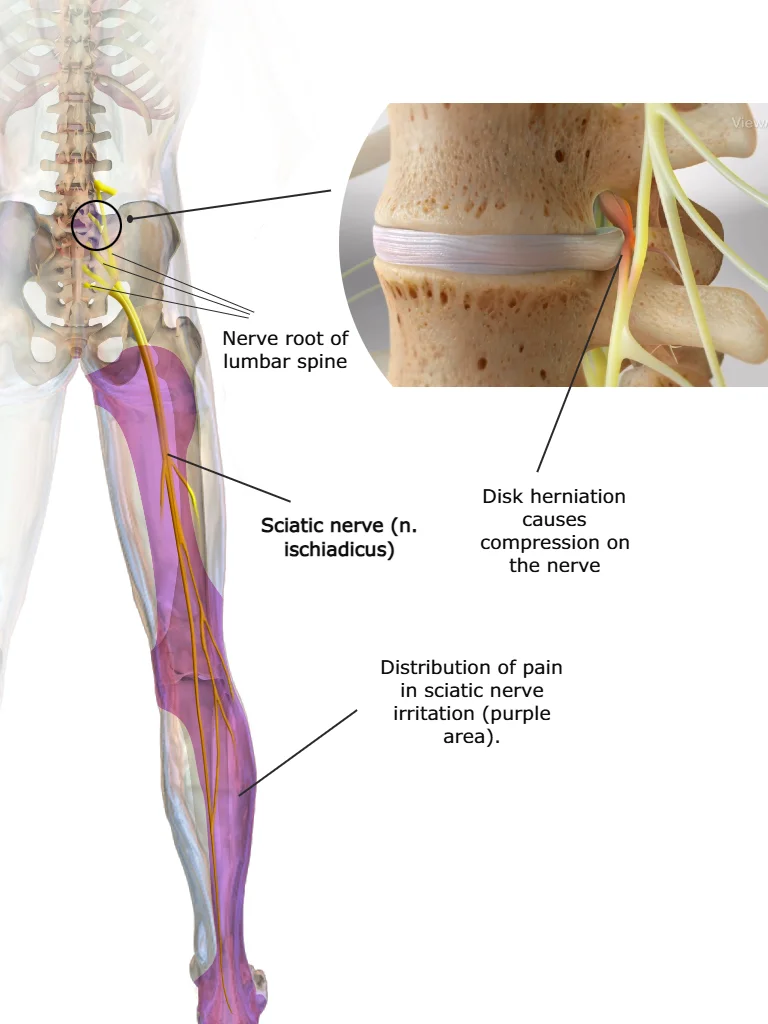
Sciatica, sometimes called lumbar radiculopathy, refers to pain that radiates from the lower back or buttock down the leg, most commonly below the knee to the foot and toes. It occurs when nerve roots in the lumbar spine that form the sciatic nerve (nervus ischiadicus) become irritated or compressed.
In addition to pain, patients may experience neurological symptoms such as muscle weakness, tingling, numbness, or changes in reflexes. In about 90% of cases, sciatica is caused by a lumbar disc herniation leading to nerve root compression. Other possible causes include spinal canal stenosis or foraminal stenosis, and more rarely tumors, cysts, or spinal infections.
Not all leg pain that radiates from the lower back is sciatica. Pain originating from spinal structures such as the facet joints or sacroiliac joints may also radiate into the leg, most often into the thigh. This type of pain is not caused by nerve compression and is referred to as referred pain.
2. What Is the Sciatic Nerve?
The sciatic nerve (nervus ischiadicus) is the largest and longest nerve in the human body. It is formed by the joining of nerve roots from the lower lumbar and upper sacral spine (L4–S3). The nerve exits the pelvis through the buttock region and travels down the back of the thigh, where it divides near the knee into branches that continue into the lower leg, foot, and toes.
The sciatic nerve plays a key role in both motor and sensory function of the lower limb. It innervates the muscles of the posterior thigh and, through its terminal branches — the tibial nerve and common peroneal (fibular) nerve — supplies most muscles of the lower leg and foot, enabling movements of the hip, knee, ankle, and foot. It also carries sensory information from the back and outer part of the lower leg and from a large portion of the foot.
3. What Causes Sciatica?
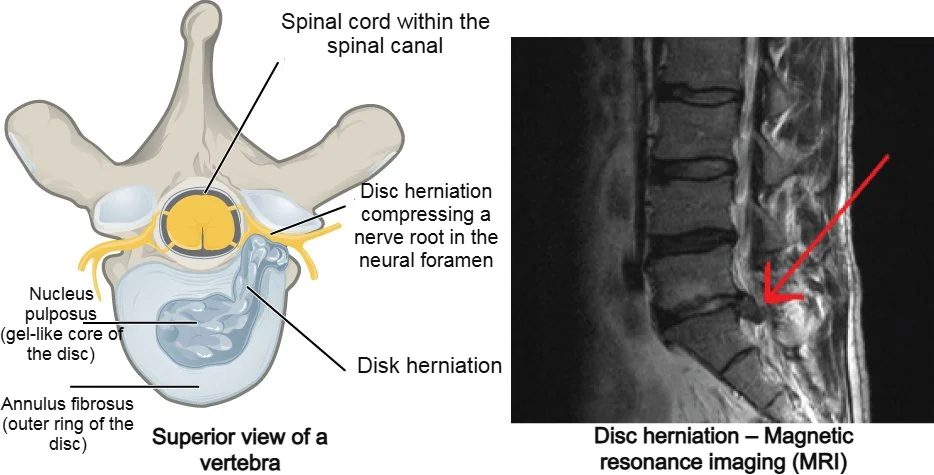
The most common cause of sciatica — particularly in younger adults — is a lumbar disc herniation or disc bulge that leads to nerve root compression or irritation. In older individuals, symptoms more often develop as a result of degenerative spine changes (spondylosis). These may include spinal canal stenosis, foraminal stenosis, formation of osteophytes (bone spurs), thickening of ligaments, and facet joint osteoarthritis, all of which can narrow the space around nerve structures and lead to irritation or compression.
Sciatica can also occur due to spondylolisthesis, where one vertebra slips forward relative to another, causing mechanical pressure on nerve roots. Less common causes include tumors, cysts, infections, or other structural abnormalities affecting the spine.
Importantly, sciatica symptoms are not caused solely by mechanical compression. They often result from a combination of mechanical pressure and inflammatory or immune-mediated processes that irritate and sensitize nerve tissue. The inner part of the intervertebral disc (the nucleus pulposus), which may protrude during disc herniation, has strong inflammatory properties when exposed to surrounding tissues. Contact with a nerve root can trigger pain, disrupt nerve signaling, and contribute to structural changes in nerve tissue.
Even mild but prolonged nerve root compression can amplify the inflammatory response by promoting the release of inflammatory mediators, further increasing nerve irritation and sensitivity.
4. What Does Sciatica Pain Feel Like –Sciatica Symptoms
The hallmark symptom of sciatica is radiating leg pain that starts in the lower back or buttock and travels down the leg, most often below the knee to the foot. Sciatica may begin suddenly — for example after physical exertion or an awkward movement — but it can also develop gradually over several days.
The pain is often severe and may significantly interfere with daily activities. Patients commonly describe it as a combination of dull and sharp pain deep in the leg, sometimes burning, tearing, or associated with a strong sense of muscle tightness in the hamstrings or calf. Symptoms are usually present for much of the day and often worsen with sitting, walking, or movements of the lumbar spine. Night pain is not uncommon and may disrupt sleep. Pain may also intensify with coughing, sneezing, or straining.
Low back pain may accompany sciatica (lumbago with sciatica), but it is not always present. When it occurs, it is often localized around the L5–S1 lumbosacral region.
A key clinical feature is that leg pain is typically more severe than low back pain.
The pattern of pain often depends on the affected nerve root:
- L5 nerve root: pain radiates down the back and outer side of the thigh and lower leg toward the top of the foot
- S1 nerve root: pain travels down the back of the thigh and calf toward the heel and sometimes the outer foot
- L4 nerve root: pain spreads along the front of the thigh to the knee and may be mistaken for hip pathology
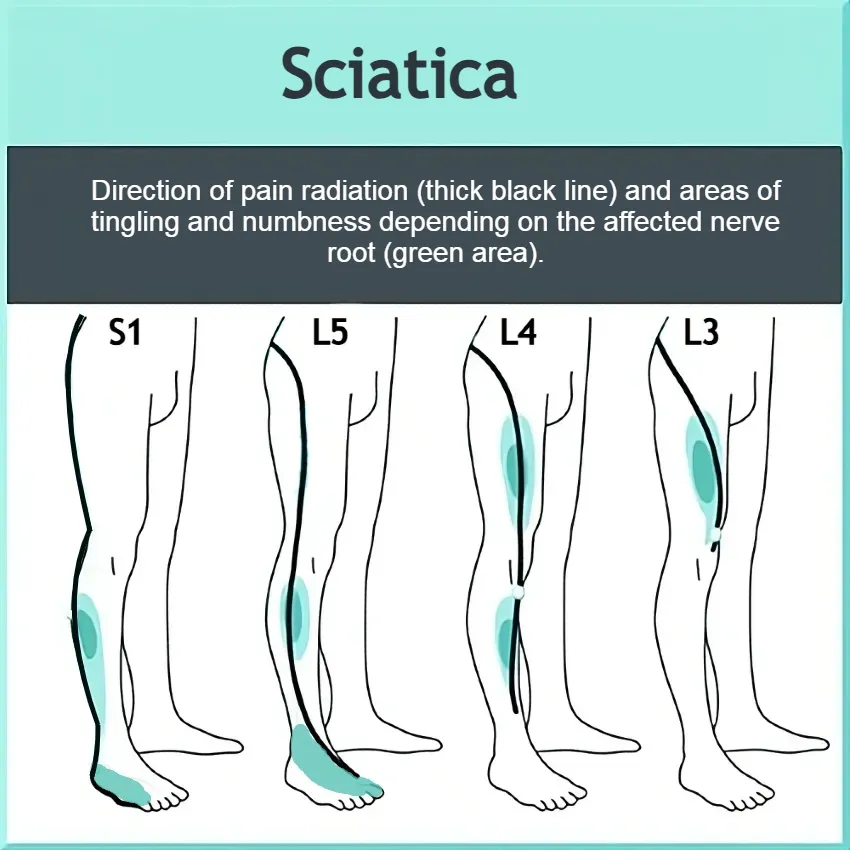
Sciatica is most commonly unilateral, although bilateral symptoms can occur with central disc herniation, lumbar spinal stenosis, or spondylolisthesis. Some patients adopt a specific posture, such as leaning forward or to one side, to reduce pressure on the affected nerve.
In addition to pain, patients may experience tingling, burning, or numbness along the nerve distribution. Muscle weakness occurs less frequently but, in rare cases, may be severe enough to cause foot drop or noticeable gait disturbance.
5. Risk Factors for Sciatica – Who Is Most at Risk?
Sciatica occurs more frequently in individuals with a history of low back pain, and its prevalence is similar in men and women. Symptoms most commonly appear between the ages of 30 and 50, while sciatica is relatively uncommon before age 20 unless associated with trauma or specific structural spinal disorders. Certain lifestyle and occupational factors may further increase the risk.
Common risk factors include:
- Previous episodes of low back pain: Individuals with recurrent lumbar pain are at higher risk of developing sciatica (lumbago with sciatica).
- Age 30–50 years: Degenerative changes of the intervertebral disc become more common and may lead to nerve root irritation or compression.
- Overweight and obesity: Increased mechanical load on the spine may accelerate lumbar disc degeneration and contribute to inflammation.
- Smoking: Associated with a higher risk of low back pain and disc degeneration; increased risk has also been observed in former smokers.
- Occupational and physical strain: Prolonged awkward postures, whole-body vibration (e.g., professional drivers), repetitive lifting, and heavy manual work increase spinal stress.
- Trauma and sudden loading: Injuries or abrupt movements that overload the lumbar spine may precipitate lumbar disc herniation or nerve root irritation.
6. How Is Sciatica Diagnosed?
The diagnosis of sciatica is primarily clinical, based on a detailed medical history and physical examination. The hallmark feature is radiating leg pain extending from the lower back or buttock down one leg, typically following the distribution of a specific nerve root (dermatome). Patients may also report paresthesia, numbness, or sensory changes.
During the neurological examination, doctors assess muscle strength, reflexes, and sensory function to identify signs of nerve root compression. One of the most widely used clinical tests is the Straight Leg Raise (Lasègue test), which helps detect nerve root irritation. The crossed straight leg raise test may also be performed and is considered more specific for lumbar disc herniation. A diagnosis is likely when typical unilateral leg pain is accompanied by neurological findings consistent with lumbar radiculopathy.
Imaging studies such as X-ray, MRI, or CT are not routinely required to establish the diagnosis. In the acute phase, imaging is recommended only when red flags suggest a serious underlying condition, such as infection, fracture, tumor, or progressive neurological deficit.
7. How to Tell if It’s Sciatica
Key signs that suggest sciatica include:
- Leg pain more intense than lower back pain
- Pain radiating toward the foot or toes
- Numbness or tingling in the same region
- Pain increases during straight leg raise (Lasègue test)
- Neurological deficit localized to a single nerve root
These features help differentiate true lumbar radiculopathy from other causes of leg or back pain.
8. When and Why to Get X-Ray or MRI for Sciatica
A common question is: Should everyone with sciatica get an X-ray or MRI? The answer is no. Most patients with sciatica never need imaging. Imaging is only useful in certain situations to confirm diagnosis or guide treatment planning.
Imaging may be needed if:
- Symptoms persist beyond a few weeks despite conservative treatment (6–8 weeks)
- There is suspicion of serious conditions such as infection, fracture, or tumor
- Significant neurological deficits appear, like marked muscle weakness or loss of bladder/bowel control
Key points about imaging:
- X-ray (radiograph) cannot show disc herniation or nerve root compression. It may reveal degenerative changes or fractures, but these often do not correlate with symptoms.
- MRI is the preferred modality when persistent pain or neurological deficits suggest a lumbar disc herniation compressing a nerve root. However, disc herniations are common even in people without symptoms (20–36% prevalence).
Takeaway:
Imaging is not routinely needed for sciatica. Even if a disc herniation is present, MRI or X-ray does not usually change treatment or speed up recovery and should always be interpreted alongside clinical findings.
9. How Long Does Sciatica Last?
Despite causing severe pain and limiting daily activities, sciatica generally has a favorable prognosis. Symptoms often improve spontaneously within a few weeks. Acute pain usually lasts 2–6 weeks, and with conservative treatment—such as rest, analgesics, and physical therapy—symptoms gradually subside.
Research shows that about 50% of patients with acute sciatica feel improvement within 10 days, and around 75% notice improvement after 4 weeks.
10. Does Sciatica Go Away?
Even without surgery, approximately 80% of patients fully recover within 8 weeks, and up to 95% recover within one year.
Overall, sciatica has a very good long-term prognosis, and surgical intervention is necessary only in a small minority of cases.
11. Sciatica Treatment
There is a consensus that the initial 6–8 weeks of sciatica management should be conservative. This primarily includes medication and physical therapy, while surgical intervention is considered only if symptoms persist or there is a significant neurological deficit.
Below, we address the most common questions regarding available treatment options.
12. What Can You Do for Sciatica Pain at Home?
For most patients with acute sciatica, simple self-care measures can provide relief and support recovery:
- Stay active: Avoid prolonged bed rest. Gentle walking and light stretching help maintain mobility and circulation.
- Posture awareness: Sitting and standing with proper lumbar support reduces pressure on the affected nerve.
- Heat and cold therapy: Applying a cold pack initially can reduce inflammation, while heat therapy can relax tight muscles.
- Over-the-counter pain relief: Short-term use of NSAIDs (e.g., ibuprofen) may help reduce discomfort, though effects are often limited.
- Gradual exercise: Simple core-strengthening or lumbar stabilization exercises can support spinal structures and prevent recurrence.
Important: Home measures are usually sufficient for mild to moderate symptoms. Seek medical advice if pain worsens, spreads, or if neurological deficits (weakness, numbness, loss of bladder/bowel control) appear.
13. Best Over‑the‑Counter Pain Reliever for Sciatica
When managing sciatica pain at home, many people first turn to over‑the‑counter (OTC) pain relievers. While no medication will eliminate sciatica instantly, some can help reduce discomfort enough to stay active and function better.
Common OTC Options
- Nonsteroidal Anti‑Inflammatory Drugs (NSAIDs):
- Ibuprofen (e.g., Advil, Motrin)
- Naproxen (e.g., Aleve)
These can help reduce inflammation and pain in the short term. However, evidence suggests that NSAIDs provide limited relief for sciatica pain in many patients.
- Acetaminophen (Paracetamol):
Acetaminophen (e.g., Tylenol) may help with general pain, but research shows minimal benefit specifically for sciatica.
What to Keep in Mind
- Use short‑term: OTC pain relievers are best for temporary relief. Long‑term use, especially of NSAIDs, can increase the risk of gastrointestinal, kidney, or cardiovascular side effects.
- Follow dosing instructions: Always use the lowest effective dose and consult a clinician if you have underlying health conditions (e.g., ulcers, kidney disease, heart issues).
- No single “best” pill: There is no universally superior OTC drug for all sciatica patients — effectiveness varies between individuals.
When to Seek Medical Advice
If OTC pain relievers don’t improve your symptoms or pain becomes severe despite proper use, speak with a healthcare provider. They may recommend other pain management strategies or adjust your treatment plan.
14. Prescription Medications for Sciatica
When over-the-counter pain relievers aren’t enough, healthcare providers may prescribe stronger medications to manage sciatica pain. Prescription options are typically reserved for moderate to severe pain or when pain interferes with daily activities.
Common Prescription Medications
- Stronger NSAIDs or COX-2 inhibitors
- Examples: Celecoxib (Celebrex)
- Used for more severe inflammation and pain when OTC NSAIDs are insufficient.
- Muscle Relaxants
- Examples: Cyclobenzaprine, Tizanidine
- Helpful for relieving muscle spasms that often accompany sciatica.
- Neuropathic Pain Medications
- Examples: Gabapentin, Pregabalin
- Target nerve-related pain, which is a key component of sciatica.
- Can reduce tingling, numbness, and shooting pain.
- Short-term Oral Corticosteroids
- Example: Prednisone taper
- Used in select cases to reduce severe inflammation around nerve roots.
- Opioids (rare cases)
- Reserved for short-term use in severe, acute pain that doesn’t respond to other treatments.
- High risk of dependence and side effects; generally avoided unless absolutely necessary.
Key Considerations
- Prescription medications are usually combined with conservative treatments like physical therapy, exercise, and lifestyle modifications.
- Always use under a doctor’s supervision due to potential side effects and drug interactions.
- Long-term use of opioids or corticosteroids is not recommended for sciatica due to safety concerns.
15. Sciatica, Walking or other Physical Activity
Many patients with sciatica wonder how much walking or exercise is safe while experiencing symptoms. Can movement worsen the condition? Strict bed rest is not recommended—in fact, it can slow recovery and prolong symptoms. Patients are encouraged to move as much as they can tolerate, and light walking or moderate physical activity usually helps maintain muscle function and circulation.
It’s important to understand that walking and gentle activity will not cause further disc displacement or additional nerve root compression. Activities like walking, mild stretching, or simple back exercises often reduce pain and speed recovery. Gradually increasing the duration and intensity of activity according to personal tolerance is recommended.
Key takeaway: Moderate activity and walking are safe and beneficial for sciatica, whereas prolonged bed rest can be harmful. The goal is to maintain mobility and function while managing pain as effectively as possible.
16. When Is Surgery Needed for Sciatica?
Fortunately, surgery is required for only a small number of sciatica patients. Most recover with conservative treatment without the need for an operation.
Absolute indications for surgery are rare and include:
- Loss of bladder or bowel control
- Progressive muscle weakness
It’s important to note that sciatica rarely causes permanent nerve or structural damage.
The most common reason for surgery is persistent pain or slow functional recovery. If symptoms last longer than 6–8 weeks despite conservative treatment, and MRI confirms a lumbar disc herniation compressing the nerve root, surgery may be considered.
The standard procedure is microdiscectomy, where a surgeon removes the portion of the herniated disc pressing on the nerve. The goal is to relieve pressure, reduce pain, and enable faster functional recovery.
Research shows that early surgery can speed recovery—symptom relief often occurs around 4 weeks after surgery, compared to approximately 12 weeks with conservative care.
Surgery provides faster symptom relief in the first few months, but the differences gradually decrease over time. After approximately one year, overall recovery is similar, with around 95% of patients recovering well regardless of the treatment approach.
Key Facts About Sciatica
- Not all leg pain is sciatica: Sciatica (lumboischialgia) is leg pain caused by irritation or compression of a spinal nerve root.
- The most common cause is a lumbar disc herniation, though symptoms can also result from degenerative spine changes or spinal canal narrowing.
- Diagnosis is usually clinical, based on symptoms and physical examination – imaging is not typically needed initially.
- Prognosis is very good: most patients notice improvement within a few weeks and recover without surgery.
- Medications have limited effect, so the focus is on movement and gradually returning to normal activities.
- Strict bed rest is not recommended – walking and moderate physical activity are safe and beneficial.
- Surgery is rarely needed and is usually considered after 6–8 weeks of unsuccessful conservative treatment or in cases of severe neurological deficit.
- Surgery can speed up recovery, but long-term outcomes after one year are similar to conservative management.
Tubach F, Beauté J, Leclerc A. Natural history and prognostic indicators of sciatica. J Clin Epidemiol. 2004 Feb;57(2):174-9. doi: 10.1016/S0895-4356(03)00257-9.
National Guideline Centre (UK). Evidence review for pharmacological management of sciatica: Low back pain and sciatica in over 16s: assessment and management. London: NICE; 2020.
Ostelo RW. Physiotherapy management of sciatica. J Physiother. 2020 Apr;66(2):83-88.
Fairag M, Kurdi R, Alkathiry A, et al. Risk Factors, Prevention, and Primary and Secondary Management of Sciatica: An Updated Overview. Cureus. 2022 Nov 12;14(11):e31405.
Valat JP, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Pract Res Clin Rheumatol. 2010 Apr;24(2):241-52.
Longo DL, Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015;372(13):1240–1248.
Cook CE, Taylor J, Wright A, et al. Risk factors for first time incidence sciatica: a systematic review. Physiother Res Int. 2014 Jun;19(2):65-78.
Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007 Oct;99(4):461-73.
Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA. Conservative treatment of sciatica: a systematic review. J Spinal Disord. 2000 Dec;13(6):463-9.
Legrand E, Bouvard B, Audran M, et al. Sciatica from disk herniation: Medical treatment or surgery? Joint Bone Spine. 2007 Dec;74(6):530-5.