Outer foot pain after running is a common complaint among runners and can significantly impact both performance and everyday mobility. The lateral side of the foot is especially vulnerable to strain from repetitive impact, poor biomechanics, or improper footwear. Whether you’re training for a marathon or jogging for general fitness, outer foot pain after running may indicate anything from overuse injuries to structural imbalances. Understanding the most common causes and how to treat them is key to recovery and injury prevention. In this article, we break down the leading reasons behind outer foot pain after running and share practical solutions to help you run comfortably again.
Anatomy of the Outer Foot
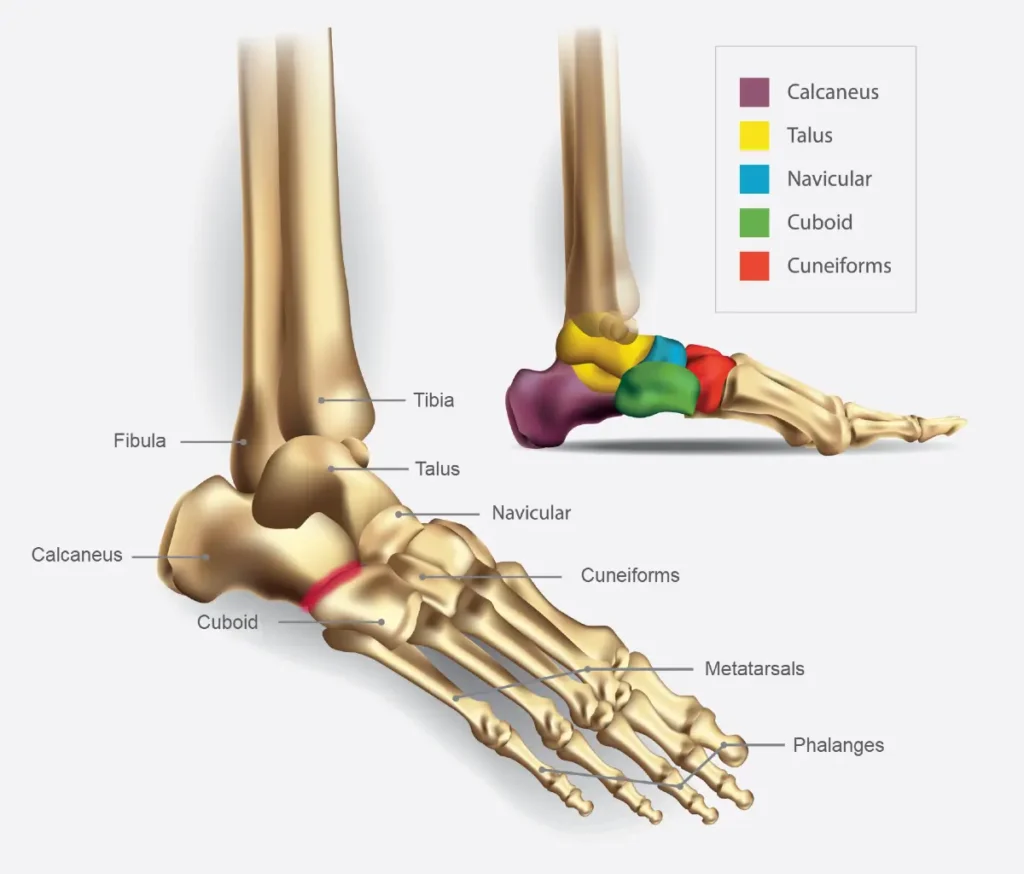
The outer part of the foot—also known as the lateral foot—is a complex structure made up of bones, tendons, ligaments, and nerves that work together to support movement and balance. Key anatomical components include:
- 5th Metatarsal Bone: Runs along the outside of the foot and is commonly affected by stress fractures or direct trauma.
- Cuboid Bone: A small bone near the middle of the lateral foot that plays a key role in foot stability and is involved in cuboid syndrome.
- Peroneal Tendons (Peroneus Longus & Brevis): These tendons run behind the outer ankle and along the side of the foot, helping with ankle stability and foot eversion.
- Lateral Ligaments of the Ankle: Especially the anterior talofibular ligament (ATFL), which can be stretched or torn during ankle sprains.
- Sural Nerve: A sensory nerve that runs down the outer leg and foot, which can be irritated in some foot or ankle conditions.
Understanding this anatomy helps identify the source of lateral foot pain after running and guides appropriate diagnosis and treatment.
What Is Outer Foot Pain?
Outer foot pain refers to discomfort or aching that occurs along the lateral (outer) side of the foot, from the base of the little toe down to the heel.
Pain on the outside of the foot is often linked to injuries or overuse of specific structures such as the peroneal tendons, fifth metatarsal bone, or cuboid bone. Because this region absorbs a significant amount of impact during lateral movements and weight transfer, it’s especially prone to strain, inflammation, or even fractures—particularly in runners or athletes with biomechanical imbalances or improper footwear.
Common Causes of Outer Foot Pain After Running
Outer foot pain after running can result from various conditions, often related to overuse, improper technique, or biomechanical issues. Below are the most common causes runners should be aware of.
1. Peroneal tendonitis
Peroneal tendonitis is a common overuse injury that affects the peroneus longus and peroneus brevis tendons, which run along the outer side of the ankle and foot. These tendons play a key role in stabilizing the foot and ankle, especially during activities that involve repetitive motion, such as running on uneven terrain or excessive pronation.
In runners, peroneal tendonitis typically develops gradually due to repetitive strain, often exacerbated by poor footwear, sudden increases in training intensity, or biomechanical imbalances like high arches. Symptoms include a dull ache or sharp pain along the outer ankle or foot, swelling, and tenderness that worsens with activity and improves with rest.
Early recognition and management are essential to prevent progression. Treatment usually involves activity modification, ice, anti-inflammatory measures, physical therapy, and proper footwear support. If untreated, chronic tendon irritation can lead to tendon degeneration or even tearing, prolonging recovery.
2. Cuboid Syndrome
Cuboid syndrome is a frequently overlooked cause of pain along the outer midfoot, particularly in runners. It results from a subtle disruption in the alignment or movement mechanics (arthrokinematics) of the calcaneocuboid (CC) joint, a key structure in lateral foot stability. This misalignment may occur gradually or following an ankle sprain, especially if the foot is forcefully inverted. In runners, it often develops due to repetitive stress, poor foot biomechanics, or training on uneven surfaces.
The pain is typically located between the heel and the base of the fourth and fifth toes, and may worsen during push-off or side-to-side movements. Symptoms can resemble those of a ligament sprain, and patients might report diffuse aching, localized tenderness, swelling, or a sense of instability in the lateral foot. Diagnosis is mainly clinical, as imaging often fails to detect the subtle joint dysfunction.
Treatment usually includes manual manipulation techniques, such as the “cuboid whip” or “cuboid squeeze,” which aim to restore joint congruence. Supportive taping, orthotic padding under the cuboid, and a temporary reduction in weight-bearing activities (like running) are often helpful. If managed early, symptoms often resolve quickly, allowing athletes to return to activity with minimal downtime.
3. Stress Fractures of the Metatarsals
Stress fractures in the metatarsal bones are a common cause of outer and forefoot pain in runners, particularly after a recent increase in training intensity or volume. These injuries most often affect the second, third, and fourth metatarsals, but proximal fourth and fifth metatarsal stress fractures can also cause pain on the outer side of the foot. A stress fracture, also known as a fatigue fracture, occurs due to repetitive overuse, where repeated microtrauma from activities like running exceeds the bone’s ability to repair itself, eventually leading to a small crack.
The pain usually starts gradually, is initially mild and intermittent, but becomes more persistent with continued running. Runners may notice mild swelling over the top of the foot and tenderness when pressing on the bone.
Diagnosis can be challenging, as X-rays are often normal in the first few weeks after symptoms appear. Subtle signs like swelling or reduced visibility of extensor tendons during toe movement may help, but MRI or bone scans are more reliable for detecting early stress injuries.
Treatment involves rest, activity modification, and sometimes temporary use of a walking boot or stiff-soled shoe to reduce stress on the bone. While central metatarsal fractures usually heal within 4 to 6 weeks, those involving the proximal fourth or fifth metatarsals may take longer and carry a risk of delayed healing or nonunion. In some cases, especially with persistent pain or poor healing, surgical options such as bone grafting and plate fixation may be discussed.
4. Os Peroneum Syndrome
Os peroneum syndrome is a less common but important cause of outer foot pain, particularly in the area just beneath the cuboid bone on the lateral plantar side. The os peroneum is a small accessory bone embedded within the peroneus longus tendon, present in a portion of the population and usually asymptomatic. However, in some cases—especially after repetitive stress or ankle inversion injuries—it can become painful due to a stress fracture, complete fracture, or separation of a multipartite os peroneum. Pain is typically localized, worsens with activity, and is often accompanied by swelling or bruising. Resisted eversion of the foot may provoke symptoms.
Diagnosis can be confirmed via X-ray, although advanced imaging like MRI or ultrasound may be needed to assess tendon involvement. Treatment usually starts conservatively, with rest, bracing, and activity modification, and in some cases corticosteroid injections. For symptomatic cases not responding to conservative care, or if the bone fragment is significantly displaced, surgical removal or repair may be required. Early recognition is key, especially in active individuals with persistent lateral foot pain following repetitive use or a minor ankle injury.
5. Tailor’s Bunion (Bunionette)
A Tailor’s bunion, or bunionette, is a bony or soft tissue prominence on the outer side of the fifth metatarsal head, often causing lateral foot pain, especially after running or wearing tight footwear. It develops gradually due to chronic pressure and friction from shoes combined with a varus alignment of the fifth toe, which pushes the toe inward and increases stress on the outer edge of the foot. Symptoms include localized tenderness, visible MTP joint deformity, redness, swelling, and sometimes thickened skin or a bursa over the area.
While X-rays are usually unnecessary unless surgery is being considered, treatment typically starts with conservative measures such as wider shoes, orthotics, protective padding (e.g., donut pads), ice, and topical NSAIDs. In persistent cases where conservative therapy fails, surgical correction can provide significant relief and improve foot alignment.
6. Ankle Instability
Chronic ankle instability is a common yet often overlooked cause of outer foot pain after running, particularly in individuals with a history of repeated ankle sprains. It typically results from ligamentous laxity or insufficient healing following previous injuries, especially of the lateral ankle ligaments such as the anterior talofibular ligament (ATFL). As a result, the ankle becomes unstable during dynamic movement, leading to altered foot mechanics and increased stress on the outer structures of the foot.
Runners may experience symptoms such as recurring pain or a feeling of “giving way” on uneven surfaces, as well as aching or sharp pain along the lateral side of the foot and ankle after activity. Over time, this instability can contribute to overuse of the peroneal tendons, irritation of the subtalar joint, or stress on the fifth metatarsal. Management includes proprioceptive training, ankle strengthening, bracing, and in persistent or severe cases, surgical stabilization may be considered to restore function and prevent further injury.
7. Improper Footwear or Running Technique
Wearing improper footwear or using poor running technique is a frequent and preventable cause of outer foot pain after running. Shoes that lack adequate lateral support, cushioning, or arch structure can lead to uneven weight distribution, increasing pressure on the outer side of the foot—especially during longer runs or on hard surfaces. Similarly, worn-out shoes may fail to absorb impact efficiently, placing additional strain on bones, tendons, and joints.
Faulty running mechanics, such as excessive supination (underpronation) or a heavy heel strike, can also shift stress toward the lateral foot and ankle. Over time, this can lead to overuse injuries such as peroneal tendonitis, stress fractures, or joint irritation. Addressing these issues through gait analysis, proper footwear selection, and technique correction—often guided by a physical therapist or running coach—can significantly reduce injury risk and improve comfort during running.
When to See a Doctor
You should consult a healthcare professional if outer foot pain persists or worsens despite rest. Key signs include:
- Pain lasting more than a few days with no improvement
- Swelling, bruising, or visible deformity
- Pain that increases with activity or interferes with walking
- Numbness, tingling, or weakness in the foot
- History of repeated ankle sprains or instability
Early diagnosis helps prevent further injury and speeds up recovery.
Diagnosis: How Outer Foot Pain After Running Is Evaluated
Accurate diagnosis of outer foot pain after running is essential for effective treatment and a safe return to activity. To begin with, the evaluation typically starts with a detailed clinical history—focusing on the onset of pain, duration, training volume, footwear, and any previous injuries. While pain that develops gradually often suggests overuse injuries like peroneal tendinopathy or stress fractures, a sudden onset following a twist or misstep may indicate ankle instability or cuboid syndrome.
Next, a physical examination helps narrow down the cause by assessing swelling, tenderness, joint mobility, and overall foot alignment. In particular, specific tests such as resisted eversion (which may trigger pain in peroneal tendonitis) or palpation along the cuboid and fifth metatarsal can be very informative. Moreover, simple manual techniques can reveal subtle joint misalignments or suggest the presence of os peroneum syndrome.
If clinical findings are inconclusive, imaging is often the next step. X-rays help rule out bone injuries, while MRI is more sensitive for detecting stress reactions or soft tissue damage. Ultrasound can also be useful for evaluating tendon integrity. Additionally, runners whose pain stems from faulty biomechanics or improper footwear may benefit from a professional gait analysis. Ultimately, a thorough evaluation ensures treatment is tailored precisely to the underlying cause—whether that’s chronic tendon stress, mechanical instability, or repetitive loading patterns.
Effective Treatment Options
Rest and Activity Modification
Reducing or pausing running is the first step toward healing. Replacing high-impact workouts with low-impact activities like swimming or cycling can maintain fitness during recovery.
Physical Therapy and Stretching
A physiotherapist can help correct biomechanical imbalances through strengthening and mobility exercises. Regular stretching of the peroneal muscles and plantar fascia can relieve lateral foot strain.
Orthotics and Footwear Adjustments
Wearing proper running shoes is crucial in preventing recurrence. Orthotics can improve alignment, redistribute pressure, and provide extra support to the outer foot.
Ice, Anti-inflammatories, and Taping
Applying ice after activity reduces inflammation, while NSAIDs help manage acute pain. Taping techniques can stabilize the foot and improve neuromuscular control during movement.
Injections or Advanced Interventions (if needed)
Corticosteroid injections may reduce inflammation in chronic cases. In rare, persistent cases, surgical options might be explored, especially for stress fractures or tendon injuries.
Preventing Outer Foot Pain in Runners
Preventing outer foot pain after running starts with a proactive approach to training, footwear, and body awareness. First and foremost, runners should avoid sudden increases in mileage or intensity—progressive loading allows the foot’s structures to adapt gradually and reduces the risk of overuse injuries like stress fractures or tendinopathies.
Equally important is investing in proper running shoes that suit your foot type and running style. Shoes should offer adequate lateral support, cushioning, and room in the toe box to prevent pressure on the outer metatarsals. Replacing worn-out shoes in time and using orthotics if needed can also make a significant difference.
In addition, focusing on strengthening and mobility—especially in the foot, ankle, and lower leg—can improve stability and reduce uneven loading during gait. Incorporating dynamic warm-ups, flexibility work, and post-run recovery routines (like stretching and self-massage) helps keep tissues resilient. Lastly, listening to your body and addressing minor discomforts early can prevent them from turning into long-term issues. With the right habits in place, most runners can stay pain-free and keep moving confidently.
Final Thoughts: Running Without Pain
Outer foot pain after running can be frustrating—but it doesn’t have to become a long-term setback. By understanding the common causes, recognizing early warning signs, and taking steps toward proper treatment and prevention, most runners can recover fully and return to pain-free movement.
Remember, every runner’s body is different. Paying attention to how your feet respond to training, choosing the right footwear, and maintaining good running mechanics can go a long way in keeping you injury-free. Stay consistent, be mindful of changes, and don’t ignore small pains—they’re often your body’s way of asking for a reset.
Walt J, Massey P. Peroneal Tendon Syndromes. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544354/
Young BA, Kniss JR, Islas F. Lateral Foot Pain in a Recreational Runner. J Orthop Sports Phys Ther. 2017 Jan;47(1):41. doi: 10.2519/jospt.2017.6941. PMID: 28042751.
Sanal HT, Chen L. Lateral Foot Pain. Skeletal Radiol. 2015 Nov;44(11):1687-8, 1705. doi: 10.1007/s00256-015-2180-y. PMID: 26031218.
Traister E, Simons S. Diagnostic considerations of lateral column foot pain in athletes. Curr Sports Med Rep. 2014 Nov-Dec;13(6):370-6. doi: 10.1249/JSR.0000000000000099. PMID: 25391092.
Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. J Orthop Sports Phys Ther. 2005 Jul;35(7):409-15. doi: 10.2519/jospt.2005.35.7.409. PMID: 16108581.
Durall CJ. Examination and treatment of cuboid syndrome: a literature review. Sports Health. 2011 Nov;3(6):514-9. doi: 10.1177/1941738111405965. PMID: 23016051; PMCID: PMC3445231.
Patel KA, Christopher ZK, Hubbard CE, O’Malley MJ. Stress Fractures of the Fifth Metatarsal in Athletes. J Am Acad Orthop Surg. 2021 Jun 15;29(12):507-517. doi: 10.5435/JAAOS-D-20-01060. PMID: 33826553.
Paavana T, Rammohan R, Hariharan K. Stress fractures of the foot – current evidence on management. J Clin Orthop Trauma. 2024 Feb 22;50:102381. doi: 10.1016/j.jcot.2024.102381. PMID: 38435398; PMCID: PMC10904895.