Medial (inner) knee pain is a frequent problem that affects both physically active individuals and those who spend much of their day sitting or standing. Although the knee joint appears simple from the outside, it is a complex structure made up of bones, cartilage, ligaments, menisci, and muscles that must work together in perfect coordination. Even minor imbalances or overload can lead to pain on the inner side of the knee.
This type of discomfort may develop gradually due to repetitive strain, poor movement patterns, or age-related changes, but it can also occur suddenly after an awkward movement or increased physical activity. Understanding why medial knee pain occurs—and which structures are involved—is essential for choosing the right treatment and preventing long-term complications.
In this guide, we explain the most common causes of medial knee pain, how to recognize warning signs, and which treatment options are supported by current medical knowledge.
Anatomy of Inner Knee
The knee is a complex joint that connects the thigh bone (femur) with the lower leg, which consists of two bones—the tibia and the fibula. The ends of each bone are covered with a layer of cartilage that absorbs shock and allows smooth movement of the joint surfaces during motion. Knee movement is generated by muscles, while ligaments and tendons are responsible for maintaining joint stability.
The inner (medial) side of the knee includes several important structures that can be a source of pain.
- The medial meniscus is a crescent-shaped cartilage structure that acts as a shock absorber between the femur and the tibia. Injury or degeneration of the medial meniscus is one of the most common causes of pain on the inner side of the knee.
- The medial collateral ligament (MCL) is a strong ligament that stabilizes the knee on the inner side and prevents the lower leg from moving outward. Strain or damage to the MCL often results in well-localized pain along the inner knee.
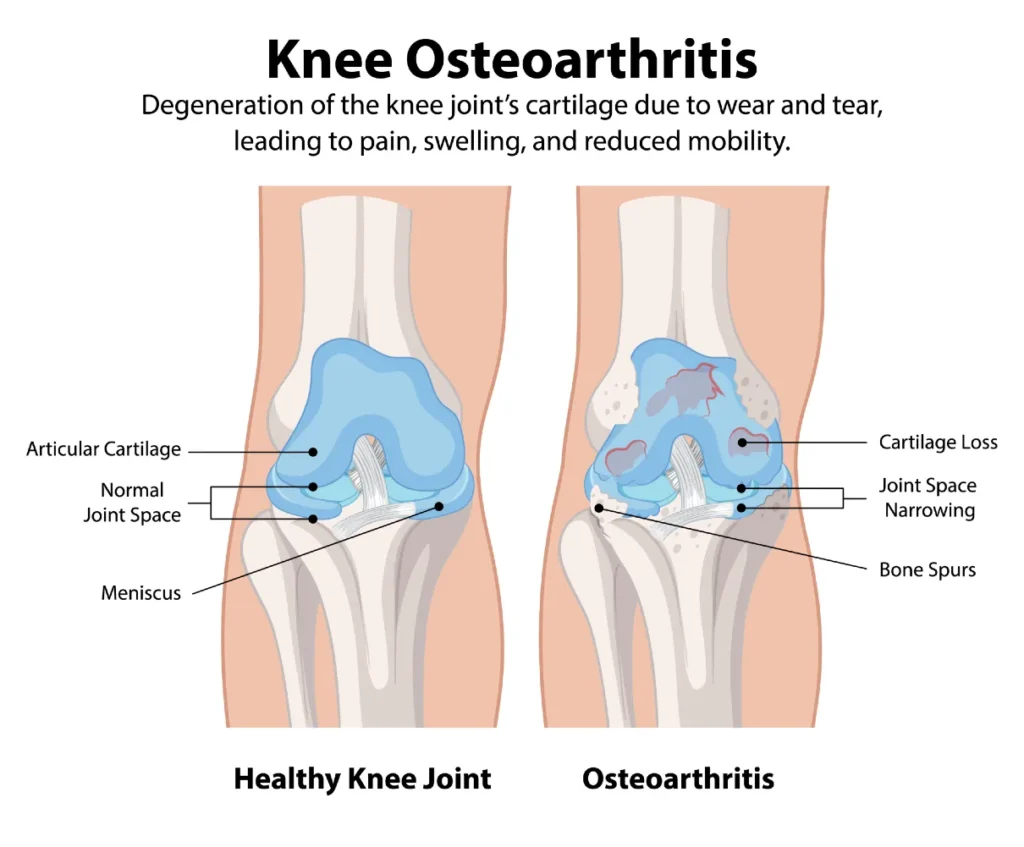
- Articular cartilage covers the ends of the bones within the knee joint and enables frictionless movement. In knee osteoarthritis, this cartilage gradually wears down—most commonly on the medial side—which can lead to pain on the inside of the knee.
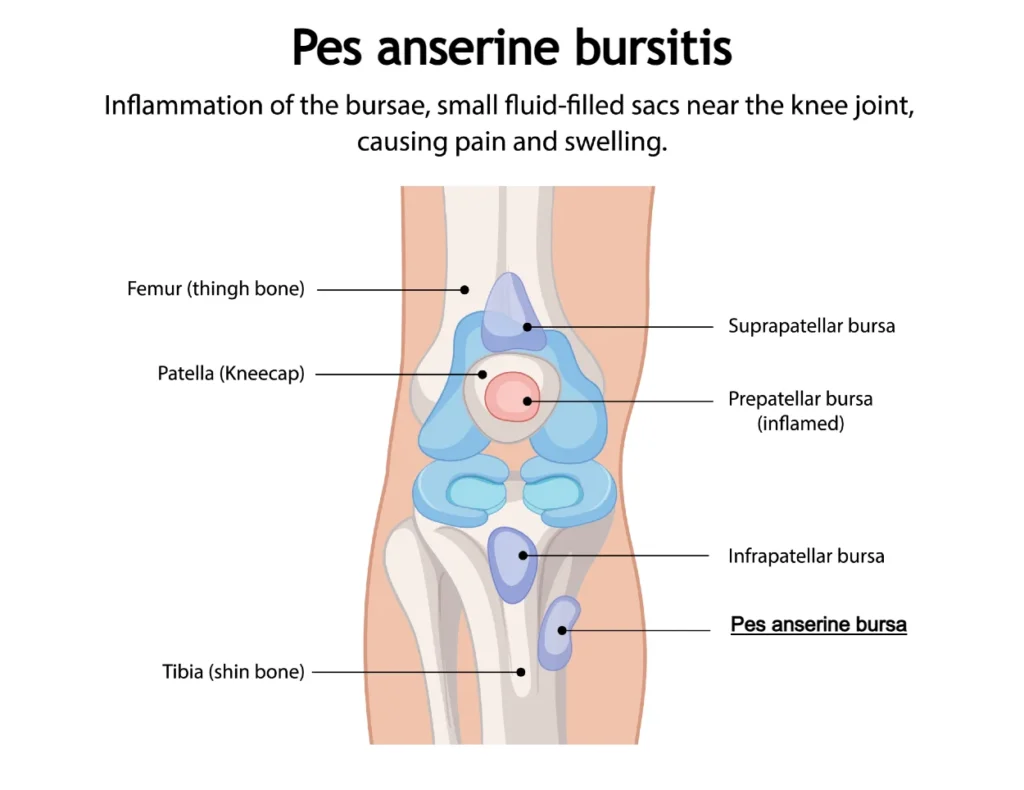
- Pes anserinus (“goose’s foot”) refers to the area where the tendons of three muscles (sartorius, gracilis, and semitendinosus) attach to the inner side of the tibia just below the knee. Inflammation in this region, known as pes anserine bursitis, is a specific and often overlooked source of medial knee pain.
Each of these structures can produce a distinct pattern of symptoms, which helps healthcare professionals identify the underlying cause of pain and choose the most appropriate treatment.
Common Causes of Medial Knee Pain
Pain on inside of knee can develop for a variety of reasons, depending on age, level of physical activity, and the presence of previous injuries. In younger individuals, the most common causes include ligament and meniscal injuries, as well as tendon inflammation related to overuse or sudden increases in activity.
In older adults, degenerative changes are by far the most frequent cause of medial knee pain. These include knee osteoarthritis and degenerative tears of the medial meniscus, which develop gradually over time rather than as a result of a single injury.
Identifying the exact cause of inner knee pain is essential for effective treatment, as different conditions require different therapeutic approaches.
Common causes of medial (inner) knee pain:
1. Knee Osteoarthritis (Gonarthrosis)
Knee osteoarthritis—also known as gonarthrosis—is a degenerative disease of the knee joint characterized by the gradual breakdown and loss of articular cartilage, accompanied by joint inflammation. As the condition progresses, the joint space narrows and bony outgrowths called osteophytes may develop. It is the most common form of knee arthritis and primarily affects older adults, which is why it is sometimes referred to as age-related arthritis.
Knee osteoarthritis is the leading cause of knee pain in people over the age of 50. In most cases, degenerative changes predominantly affect the inner (medial) compartment of the knee, making medial knee pain significantly more common than pain on the outer side.
Symptoms
The main symptom of knee osteoarthritis is pain that typically develops gradually over months or years and is often more pronounced on the inner side of the knee. Pain is usually triggered or worsened by weight-bearing activities such as walking, especially when climbing stairs or walking uphill, as well as kneeling. Rest usually provides symptom relief.
In later stages of the disease, knee pain may also occur at rest. As osteoarthritis progresses, symptoms tend to intensify and may include joint stiffness, difficulty walking or climbing stairs, and occasional inflammatory flare-ups accompanied by knee swelling.
Diagnosis
The diagnosis of knee osteoarthritis is based on a combination of typical symptoms, the patient’s age, clinical examination, and imaging findings. X-ray imaging of the knee is the most commonly used diagnostic method, as it allows assessment of the severity of osteoarthritis and identification of structural joint changes.
Treatment
Treatment of knee osteoarthritis usually begins with non-surgical approaches aimed at reducing pain and improving joint function. Initial management typically includes physiotherapy to strengthen surrounding muscles and improve mobility, the use of pain-relieving medications, and knee braces to enhance joint stability.
When necessary, injection therapies such as corticosteroids, hyaluronic acid, or platelet-rich plasma (PRP) may be used to further reduce inflammation and relieve symptoms.
If conservative treatments fail to provide sufficient relief and pain or limited mobility significantly interfere with daily activities, surgical options may be considered. The most common surgical procedure is total knee replacement, which can lead to substantial pain reduction and restoration of functional movement.
Learn more about knee osteoarthritis: For a comprehensive guide on causes, symptoms, diagnosis, and treatment of knee osteoarthritis, Gonarthrosis (Knee Osteoarthritis): Causes, Symptoms and Treatment
2. Medial Meniscus: Acute and Degenerative Tears
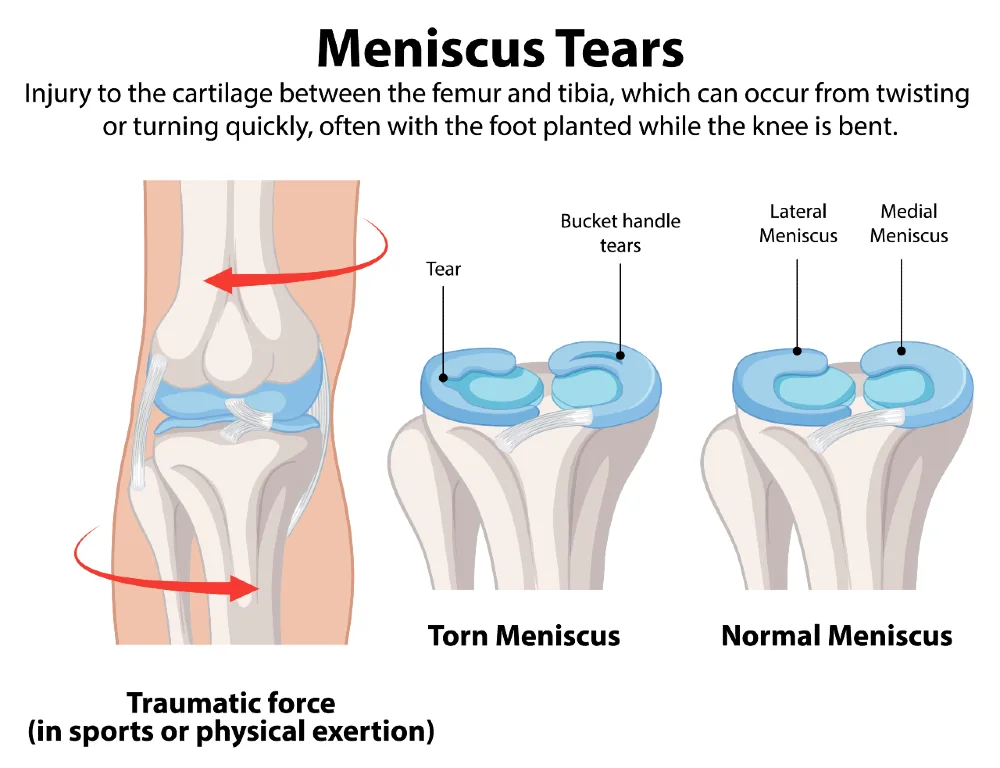
The knee meniscus is a crescent-shaped cartilage structure located between the joint surfaces of the femur and tibia. There are two menisci in each knee: the medial meniscus on the inner side of the knee, and the lateral meniscus on the outer side.
Meniscus tears are among the most common knee injuries and a frequent cause of pain on inside of knee. Tears can result from acute trauma or develop gradually due to degenerative changes over time. The risk of meniscus injury increases with age, in individuals with excess body weight, and in those with knee osteoarthritis.
Acute meniscus tears occur more often in people under 40 and are usually associated with sports activities. Sports that involve sudden changes in direction or rotation of the knee—such as soccer, handball, basketball, and skiing—pose a higher risk. Acute meniscus injuries are often accompanied by damage to the anterior cruciate ligament (ACL).
Degenerative tears are more common in individuals over 40. Over time, the meniscus loses elasticity and becomes weaker, making it less resistant to mechanical stress. Degenerative meniscus tears are frequently associated with knee osteoarthritis. In these cases, even minor twisting of the knee—such as when standing up from a chair—can cause a tear. Up to half of meniscus injuries in older adults occur spontaneously, with patients often unaware of any specific injury.
Symptoms of Medial Meniscus Tears
The main symptom of a medial meniscus tear is pain on the inner side of the knee. In acute injuries, symptoms appear immediately or within 1–3 days after trauma. Degenerative tears usually cause gradual pain without a clear traumatic event.
Other common symptoms include:
- Swelling that worsens with activity
- Mechanical issues such as clicking, locking, or a feeling of instability
- In some cases, a fragment of the meniscus can become trapped in the joint, causing complete knee blockage
Not every meniscus tear causes symptoms. In fact, tears are often found incidentally on MRI scans, with prevalence increasing with age. Up to 60% of individuals with a meniscus tear on MRI may have no complaints at all.
Diagnosis
On physical examination, swelling and localized medial knee tenderness are often present. Clinicians use specific tests such as the Thessaly test, McMurray test, and Apley test to help identify tears. MRI is the most accurate imaging method for detecting meniscus tears, while X-rays and ultrasound are less useful for this purpose.
Treatment
Initial management of acute meniscus injuries involves rest, elevation, and ice to reduce pain and swelling. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or diclofenac, may help during the acute phase. Once symptoms subside over a few weeks, physiotherapy is recommended to restore strength and mobility.
If pain, swelling, or mechanical symptoms persist after physiotherapy, surgical intervention may be considered. This can include meniscus repair (suturing) or partial removal (meniscectomy). Repairing the meniscus is preferred whenever possible, as meniscectomy increases the risk of accelerated knee osteoarthritis.
Learn more about meniscus injuries: For a detailed guide on causes, symptoms, diagnosis, and treatment of medial and lateral meniscus tears, Meniscal Tears: Symptoms, Diagnosis and Recovery
3. Medial Collateral Ligament (MCL) Injury
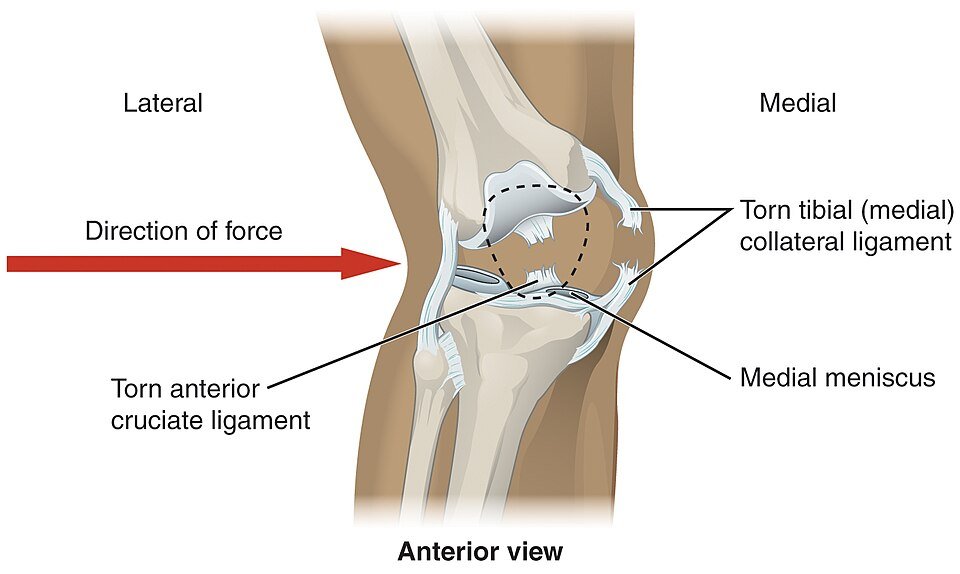
The medial collateral ligament (MCL) is a flat band of connective tissue that runs along the inner side of the knee, connecting the femur (thigh bone) to the tibia (shin bone). Its primary function is to provide lateral stability to the knee, preventing excessive outward deviation of the lower leg.
MCL injuries are common in sports, particularly in contact sports and skiing. Interestingly, up to 60% of skiing-related knee injuries involve the MCL. After the anterior cruciate ligament (ACL), MCL injuries are the second most common ligamentous knee injury.
Mechanism of Injury
MCL injuries most often occur in young and middle-aged adults, especially athletes and recreational sports participants. These injuries are associated with activities involving sudden twisting, directional changes, or rotational movements of the knee. A direct blow to the outer side of the knee is another common mechanism, frequently seen in contact sports such as soccer, handball, and rugby.
MCL injuries can occur in isolation, but often other knee structures are affected simultaneously. A well-known example is the “unhappy triad,” which involves concurrent injury to the MCL, ACL, and medial meniscus. Due to the complexity of these injuries, early recognition and appropriate treatment are crucial for maintaining knee stability and function.
Symptoms
Individuals with an MCL injury often report pain on the inner side of the knee (medial knee pain), which may appear acutely or develop gradually. In acute injuries, pain usually occurs immediately following trauma, most often during sports or sudden movements. Some patients describe a “popping” sensation at the moment of injury, followed by difficulty walking and a feeling of instability.
In more severe cases, particularly with complete MCL tears, swelling along the inner side of the knee is common. These symptoms are important indicators of injury severity and often require thorough diagnostic evaluation.
Diagnosis
The diagnosis of an MCL tear is based on clinical examination and imaging, such as ultrasound or MRI. Swelling and bruising may be observed on the inner side of the knee, while direct-impact injuries can also cause bruising on the outer side. The valgus stress test is a key clinical maneuver used to assess MCL integrity and knee stability.
MRI is considered the gold standard for evaluation, providing detailed visualization of the ligament and detecting any associated injuries, such as ACL or meniscus damage. Ultrasound offers a faster and more accessible alternative and allows real-time assessment of ligament integrity during a valgus stress test.
Treatment
Most MCL injuries are treated conservatively, especially mild cases. Management includes pain relief with analgesics, short-term immobilization, and a gradual physiotherapy program focused on strengthening the thigh and hip muscles to stabilize the knee.
In more severe injuries, particularly those with associated ACL or meniscus tears, or in athletes with persistent knee instability, surgical intervention may be considered.
4. Pes Anserinus Bursitis
The term “pes anserinus” literally translates from Latin as “goose’s foot.” It refers to the area where the tendons of three muscles—the sartorius, gracilis, and semitendinosus—attach to the tibia on the inner side of the lower leg, just below the knee. Between these tendons and the medial collateral ligament lies a small fluid-filled sac called a bursa, which allows the tendons to glide smoothly. Irritation of this bursa can lead to inflammation and fluid accumulation, resulting in a painful condition known as pes anserinus bursitis.
Pes anserinus bursitis most commonly occurs in middle-aged adults, particularly women, often with excess body weight. Main symptom is medial knee pain. It is frequently seen in individuals who already have an underlying knee problem, such as knee osteoarthritis, meniscus injury, or genu valgum (knock knees). Unlike other overuse syndromes, it is less common in highly active individuals, though physical activity can still exacerbate irritation and inflammation.
Symptoms
Patients typically report sharp, stabbing pain on the inner (medial) side of the knee, especially when rising from a chair, climbing stairs, or sitting with crossed legs. The painful area is located about five centimeters below the knee joint and is tender to touch. In some cases, mild swelling and redness may be present.
Diagnosis
Pes anserinus bursitis is usually diagnosed based on clinical examination alone, without the need for additional imaging, unless symptoms are atypical or the case is complex. In such situations, ultrasound or MRI can help assess the condition of the bursa and the hamstring tendons.
Treatment
Pes anserinus bursitis often resolves on its own with rest, analgesics, and cold compresses. If symptoms persist, physiotherapy is recommended, including strengthening and stretching exercises for the hamstrings and therapeutic modalities such as laser therapy, ultrasound, or shockwave therapy. Pain can also be managed with ultrasound-guided corticosteroid injections if needed. Surgical treatment is rarely required.
5. Inflammatory Conditions Affecting the Knee (Rheumatoid Arthritis, Gout, etc.)
Inflammatory arthritides and systemic diseases are a group of disorders characterized by chronic joint inflammation and involvement of other organs, often caused by autoimmune processes or crystal deposition.
The most well-known autoimmune inflammatory disease is rheumatoid arthritis (RA), while the most recognized crystal-induced arthritis is gout. Both conditions frequently affect the knee, causing pain and swelling. In these cases, medial knee pain can often be the most pronounced symptom.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic autoimmune inflammatory disease that primarily affects synovial joints, including the knee. An abnormal immune response leads to joint inflammation and the formation of pathological tissue called pannus, which gradually destroys cartilage and bone.
Symptoms include:
- Pain and swelling
- Joint stiffness, especially in the morning
- Reduced range of motion
In the knee, inflammation can cause noticeable swelling and warmth over the joint. Treatment typically involves disease-modifying antirheumatic drugs (DMARDs), biologic therapies, anti-inflammatory medications, and physiotherapy. In cases of localized inflammation, intra-articular corticosteroid injections may also be used.
Gout
Gout is an inflammatory arthritis caused by the deposition of uric acid crystals in joints, leading to severe pain and swelling, most commonly in the knee or the big toe joint. It primarily affects adults, especially older men. Attacks typically begin suddenly and are accompanied by redness and warmth over the affected joint.
Diagnosis is made through synovial fluid analysis and elevated blood uric acid levels. Treatment includes medications to reduce inflammation during attacks, long-term therapy to control uric acid levels, and lifestyle modifications such as dietary changes and exercise.
6. Less Common Causes of Medial Knee Pain
In addition to the more frequent causes, inner knee pain can also result from less common conditions such as avascular necrosis (AVN) of the bone or spontaneous subchondral fracture of the knee (SIFK). These conditions can cause localized pain and difficulty moving the joint.
Bone marrow edema may also lead to significant knee pain and often occurs as a result of injury or overuse. Another less common cause is plica syndrome, which arises from irritation of a fold in the synovial membrane inside the knee, leading to pain and a catching or locking sensation within the joint.
Although these causes are rare, it is important to recognize them, as they require a specific diagnostic and treatment approach. Therefore, in cases of persistent or unusual knee pain, a thorough examination and additional imaging studies are recommended.
What to Do if You Experience Pain on the Inside of the Knee?
Whether your knee pain is due to an injury, overuse, or underlying conditions such as osteoarthritis, there are several steps you can take to help relieve discomfort and support recovery. Simple self-care measures can often reduce pain, improve mobility, and prevent further aggravation of the joint.
If the pain does not improve within 7–14 days despite following self-care measures, it is best to see a doctor to determine the underlying cause of the knee pain.
How Are Medial Knee Pains Diagnosed?
Diagnosing medial (inner) knee pain is essential for selecting the correct treatment and ensuring a faster recovery. The process typically involves a thorough medical examination, symptom assessment, and appropriate imaging studies to determine the exact cause of the pain.
If you have experienced a knee injury and inner knee pain persists for several days despite self-care measures, you should seek urgent evaluation at an orthopedic or trauma clinic. An X-ray can reveal bone trauma, while a knee MRI may be required if a tear of the medial meniscus or medial collateral ligament (MCL) is suspected.
If the inner knee pain occurs without prior injury, it is more likely due to a chronic condition such as knee osteoarthritis or pes anserinus bursitis. These conditions are usually managed by a physiatrist. In such cases, X-rays may be performed to assess the degree of gonarthrosis, and ultrasound can help confirm pes anserinus bursitis.
When an inflammatory condition such as rheumatoid arthritis or gout is suspected, laboratory tests are necessary to confirm the diagnosis and guide treatment.
When to Seek Medical Help for Medial Knee Pain
Although most cases of inner knee pain can be managed with self-care measures, there are situations when it is important to consult a healthcare professional. Seek medical attention if you experience any of the following:
- Pain persists for several weeks despite rest and home care.
- Pain worsens or intensifies over time.
- Noticeable swelling, redness, or warmth around the knee.
- Knee instability, a feeling of “giving way,” or inability to bear weight normally.
- Limited range of motion, making it difficult to fully bend or straighten the knee.
- Clicking, popping, or locking of the joint during movement.
- Fever or general symptoms such as weakness and fatigue, which may indicate inflammation or infection.
- A history of a serious injury (fall, blow, or sports trauma) after which knee pain is severe and persistent.
In cases where ligament tears, meniscus injury, or fractures are suspected, it is crucial to seek evaluation from a specialist immediately.
Conclusion
Medial knee pain can arise from a variety of causes, ranging from overuse and minor injuries to chronic conditions or inflammatory diseases. Most cases improve with self-care measures such as rest, gradual loading, cold therapy, compression, elevation, and targeted exercises.
However, persistent, worsening, or severe pain should not be ignored, as it may indicate a more serious underlying condition that requires medical evaluation. Early diagnosis and appropriate treatment can prevent further damage, improve function, and reduce the risk of long-term complications.
Remember to listen to your body, follow preventive measures, and consult a healthcare professional if symptoms do not improve or if you experience any red flags.
Raj MA, Bubnis MA. Knee Meniscal Tears. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [Updated 2023 Jul 17]. Available from: NCBI StatPearls
:contentReference[oaicite:0]{index=0}Mass H, Katz JN. The influence of meniscal pathology in the incidence of knee osteoarthritis: a review. Skeletal Radiology. 2023 Nov;52(11):2045–2055. Available from: PubMed
:contentReference[oaicite:1]{index=1}Irfan Atik I, Gul E, Atik S. Evaluation of the relationship between knee osteoarthritis and meniscus pathologies. Malawi Med J. 2024 Mar;36(1):48–52. Available from: PubMed
:contentReference[oaicite:2]{index=2}Pes Anserine Bursitis. StatPearls – NCBI Bookshelf. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: NCBI StatPearls
:contentReference[oaicite:3]{index=3}Nur H, Aytekin A, Gilgil E. Medial collateral ligament bursitis in a patient with knee osteoarthritis: a case report. J Back Musculoskelet Rehabil. 2018;31(4):589–591. Available from: PubMed
:contentReference[oaicite:4]{index=4}Yagi S, Sata M. Rupture of pes anserine bursa in a patient with pes anserine pain syndrome due to osteoarthritis. J Med Invest. 2019;66(1.2):211–212. Available from: PubMed