Arthritis in the hips, also known as hip osteoarthritis or coxarthrosis, is a common degenerative joint disease, often referred to as “wear-and-tear” arthritis. It primarily affects older adults and is one of the largest weight-bearing joints in the body, second only to the knee in susceptibility.
Hip arthritis gradually leads to pain, stiffness, and reduced range of motion, which can significantly impact daily activities such as walking, climbing stairs, or getting up from a chair. The condition involves the progressive breakdown of cartilage, inflammation of the joint lining (synovium), and the formation of hip bone spurs (osteophytes).
Understanding the early symptoms of hip arthritis is crucial for timely diagnosis and management. Early recognition can help reduce pain, maintain mobility, and improve quality of life. This article provides a comprehensive guide to arthritis in hips symptoms, risk factors, diagnosis, and treatment options.
Hip Anatomy (Brief)
The hip is a ball-and-socket synovial joint, one of the largest weight-bearing joints in the human body. It consists of the femoral head (the ball) and the acetabulum of the pelvis (the socket). This design provides both stability and a wide range of motion, allowing you to walk, run, bend, and rotate your legs.
The joint surfaces are covered with smooth cartilage, which reduces friction and absorbs shock. Around the edge of the acetabulum is the labrum, a ring of fibrocartilage that deepens the socket and adds stability. The hip is also surrounded by strong ligaments and a joint capsule, protecting it from dislocation while permitting movement in multiple directions.
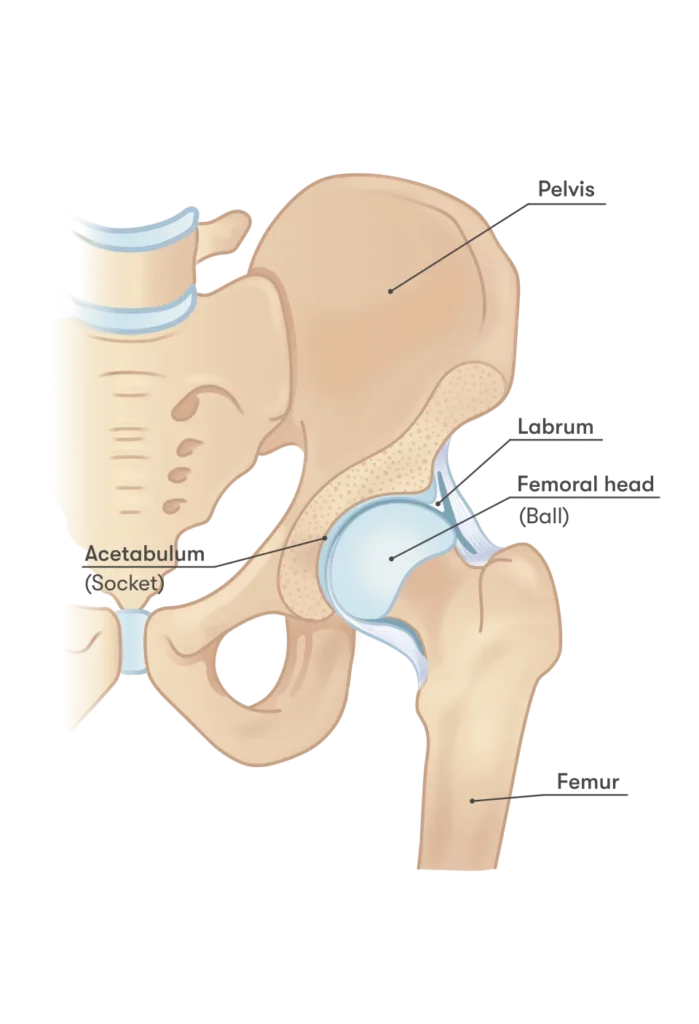
Inside the joint, synovial fluid lubricates the surfaces and nourishes the cartilage. Healthy cartilage and synovial fluid are essential for pain-free movement. When this balance is disrupted—due to wear-and-tear, injury, or inflammation—it can lead to hip arthritis, causing pain, stiffness, and limited mobility.
Why it matters for symptoms: Understanding the hip’s structure helps explain why arthritis causes deep groin pain, stiffness, and difficulty with daily activities like walking or climbing stairs.
What is Hip Arthritis (Osteoarthritis)
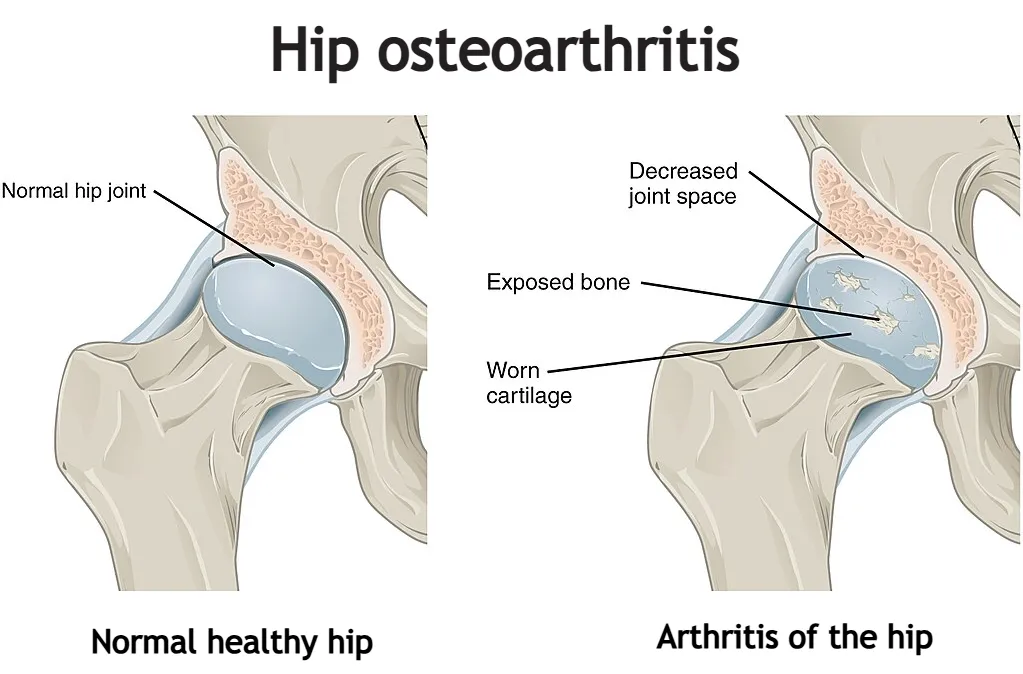
Hip arthritis, also called hip osteoarthritis (OA) or coxarthrosis, is a progressive joint disease that affects not only the cartilage but the entire hip joint. It develops due to a combination of mechanical and biochemical factors, including repeated stress, joint deformities, and the release of inflammatory molecules that disrupt normal tissue metabolism.
Early changes occur at the molecular level, leading to cartilage softening, loss of elasticity, and eventual damage. As cartilage wears away, the underlying bone becomes exposed, joint space narrows, and bone spurs (osteophytes) may form. Inflammation of the synovial membrane further contributes to pain, stiffness, and reduced mobility. Hip osteoarthritis is therefore a complex, whole-joint disease that gradually impairs function and quality of life.
Prevalence and Risk Factors
Hip osteoarthritis is a common condition, especially among older adults. Studies show that over 9% of people aged 45 and older are affected, with women slightly more likely than men to develop the disease. Lifetime risk is estimated at 18.5% for men and 28.6% for women. With an aging population and rising obesity rates, the number of people affected by hip arthritis continues to increase.
Key Risk Factors
- Age – The risk of hip arthritis rises significantly after age 45.
- Sex – Women are more prone after age 50, possibly due to postmenopausal changes.
- Genetics – A family history of hip osteoarthritis increases your likelihood of developing the condition.
- Obesity – Excess weight places added stress on the hip joint and contributes to inflammation.
- Previous Hip Injuries – Fractures or dislocations can lead to early degeneration.
- Developmental Abnormalities – Conditions such as hip dysplasia can predispose to arthritis later in life.
- Occupation and High-Impact Sports – Jobs or activities involving repetitive stress, heavy lifting, or high-impact movement may increase risk.
Understanding these factors helps identify individuals at higher risk and emphasizes the importance of early detection. Awareness allows for lifestyle adjustments, preventive care, and timely medical evaluation to slow progression and manage symptoms effectively.
Arthritis in Hips Symptoms
Hip arthritis often develops gradually, and symptoms can vary from mild discomfort to significant pain that limits daily activities. Recognizing the early signs is essential for timely intervention.
1. Hip Pain
The most common symptom is deep pain in the hip, often felt in the groin area, outer thigh, or sometimes radiating down to the knee. Pain usually worsens with activity such as walking, climbing stairs, or standing for long periods, and may improve with rest. In advanced stages, pain can occur even at rest or during sleep.
2. Stiffness
Stiffness is typically most noticeable in the morning or after periods of inactivity. Patients may have difficulty bending, rotating, or fully extending the hip. This stiffness can make routine activities, such as getting out of a chair, putting on shoes, or climbing stairs, challenging.
3. Limited Range of Motion
As arthritis progresses, movement in the hip joint becomes restricted. Internal rotation, flexion (bending), and adduction (moving the leg inward) are often most affected. Limited mobility contributes to changes in gait and can cause compensatory stress on other joints.
4. Functional Limitations
Hip arthritis impacts daily life. Walking long distances, standing for prolonged periods, or performing household tasks can become painful. Some patients notice a limp or altered gait due to pain or muscle weakness around the hip.
5. Audible Sounds and Sensations
Some individuals experience clicking, grinding, or “locking” sensations in the hip, caused by cartilage fragments or changes in joint mechanics. While these are not always painful, they indicate underlying joint degeneration.
Key Takeaway:
Early recognition of hip pain, stiffness, and reduced mobility can prevent further joint damage and allow for timely management. Patients experiencing these symptoms should consult a healthcare professional for evaluation.
Diagnosis of Hip Arthritis
Diagnosing hip arthritis is based on a combination of clinical evaluation and imaging studies. Symptoms and physical findings are often present before significant changes appear on imaging, so diagnosis does not rely on X-rays alone.
Clinical Examination
The diagnostic process begins with a detailed medical history and physical examination. A healthcare provider will ask about:
- Location and duration of hip pain
- Stiffness, especially in the morning or after rest
- Limitations in daily activities such as walking or climbing stairs
During the physical exam, the clinician assesses range of motion, gait, muscle strength, and pain response during hip movement. Reduced internal rotation and flexion of the hip are common findings in arthritis.
X-ray Imaging
X-rays are the first-line imaging tool for suspected hip arthritis. They help confirm the diagnosis and assess the severity of joint damage. Typical X-ray findings may include:
- Narrowing of the joint space
- Hip bone spurs (osteophytes)
- Changes in bone structure beneath the cartilage

It is important to note that symptoms may exist even when X-ray findings are mild or absent, especially in early disease.
MRI and Ultrasound
Advanced imaging is not routinely required, but may be used in selected cases:
- MRI provides detailed images of cartilage, bone marrow, labrum, and surrounding soft tissues. It is useful when symptoms are unexplained or when other conditions such as labral tears or avascular necrosis are suspected.
- Ultrasound can detect joint effusion and inflammation and is often used to guide diagnostic or therapeutic injections.
Key Point
A normal X-ray does not rule out hip arthritis. Diagnosis is based on symptoms, physical examination, and imaging findings together, ensuring accurate assessment and appropriate treatment planning.
Treatment Options: How to Ease Pain in Hip Arthritis
Although hip arthritis cannot be cured, a combination of conservative and surgical treatment options can significantly reduce symptoms and improve quality of life. The main goal of treatment is to ease pain in the hip, maintain mobility, and slow disease progression.
Conservative Treatment (Non-Surgical Options)
For most patients, treatment begins with non-surgical strategies focused on pain relief and function.
Exercise and Physical Therapy
Regular, low-impact exercise is one of the most effective ways to ease pain in hip arthritis. Targeted exercises help:
- Strengthen the muscles surrounding the hip
- Improve flexibility and range of motion
- Reduce joint stiffness and improve stability
Recommended activities include walking, cycling, swimming, water-based exercises, yoga, and Pilates. High-impact activities such as running or jumping should be avoided.
Weight Management
Excess body weight increases stress on the hip joint. Even modest weight loss can significantly reduce hip pain and improve mobility by decreasing joint load and inflammation.
Medications
Pain-relieving medications may help manage symptoms:
- Paracetamol (acetaminophen) for mild pain
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen for pain and inflammation
Medications should be used at the lowest effective dose and for the shortest duration possible due to potential side effects.
Injections
When pain persists despite other measures, injections may be considered:
- Corticosteroid injections to reduce inflammation and pain temporarily
- PRP (platelet-rich plasma) or hyaluronic acid injections are sometimes used, but evidence for long-term benefit in hip arthritis remains limited
Due to the depth of the hip joint, injections are typically performed under ultrasound or X-ray guidance.
Surgical Treatment
Surgery is considered when conservative treatments fail to ease hip pain and symptoms significantly affect daily life.
Total Hip Replacement (THR)
Total hip replacement is the most effective surgical option for advanced hip arthritis. The damaged joint is replaced with an artificial implant, resulting in:
- Significant pain relief
- Improved mobility and function
- High long-term success rates
More than 90% of patients experience substantial improvement after surgery, with modern implants lasting 15–25 years or longer.
Lifestyle, Self-Care, and Management
Managing hip arthritis effectively goes beyond medical treatments—it also involves adopting healthy lifestyle habits and self-care strategies. These measures can help ease hip pain, maintain mobility, and improve overall quality of life.
1. Regular Low-Impact Exercise
Engaging in low-impact activities such as walking, swimming, cycling, or yoga strengthens the muscles around the hip joint, improves flexibility, and reduces stiffness. Regular exercise not only helps maintain mobility but also supports joint stability, which is crucial for preventing further degeneration.
2. Weight Management
Maintaining a healthy weight can significantly reduce stress on the hip joint. Even modest weight loss decreases the load on your hips during daily activities, which can ease pain and slow the progression of arthritis. Combining a balanced diet with regular exercise is the most effective strategy.
3. Stretching and Flexibility
Incorporating gentle stretching exercises into your daily routine helps preserve the range of motion in the hip joint. Stretching can relieve stiffness, improve circulation, and prevent secondary problems such as muscle imbalances or poor posture caused by compensating for hip pain.
4. Use of Supportive Aids
Walking aids like canes or crutches can reduce joint load and improve stability during movement. Properly adjusted aids can make walking less painful, allowing you to remain active and independent.
5. Pain Management Strategies
Following prescribed medical guidance is essential for controlling hip pain. This may include taking medications as directed, attending physical therapy sessions, and using heat or cold therapy to alleviate discomfort. Learning techniques for pacing activities and avoiding overexertion can also help reduce flare-ups.
6. Incorporating Rest and Recovery
Balancing activity with adequate rest is crucial. Avoid prolonged periods of inactivity, but also ensure that your hip joint has time to recover after exercise or daily tasks. Short breaks and proper posture while sitting can prevent additional strain on the hip.
Conclusion:
Combining these self-care strategies with medical treatment offers the best chance of maintaining hip function and minimizing discomfort. Patients who actively manage their lifestyle, exercise safely, and follow medical guidance often experience improved mobility, less pain, and better overall quality of life.
Prognosis / Long-Term Outlook
Hip arthritis is a chronic, progressive condition, but outcomes vary depending on severity, treatment, and lifestyle:
- Conservative Management: Many patients maintain function and mobility for years with exercise, weight management, medications, and lifestyle adjustments.
- Surgical Intervention: Total hip replacement offers excellent long-term outcomes, with most patients experiencing significant pain relief and restored mobility.
- Progression: Without intervention, arthritis can worsen gradually, leading to reduced range of motion, muscle weakness, and functional limitations.
A proactive approach combining medical care, exercise, and self-management improves the long-term outlook and quality of life.
Patient Tips / Daily Life Adaptations
Practical strategies can help patients live comfortably with hip arthritis:
- Plan Activities: Pace tasks and take breaks to avoid overloading the hip joint.
- Home Adjustments: Use supportive chairs, cushions, or handrails to reduce strain.
- Exercise Routine: Incorporate gentle stretching and strengthening exercises daily.
- Footwear: Wear cushioned, supportive shoes to absorb impact.
- Assistive Devices: Canes or walkers can enhance stability and reduce pain.
- Pain Management: Apply heat/cold, follow prescribed medications, and listen to your body.
Small, consistent adaptations can make daily life more manageable while protecting joint health.
Hutton CW. Osteoarthritis: the cause not result of joint failure? Ann Rheum Dis. 1989 Nov;48(11):958-61. doi: 10.1136/ard.48.11.958. PMID: 2688566; PMCID: PMC1003922.
Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA. Hip Osteoarthritis: A Primer. Perm J. 2018;22:17-084. doi: 10.7812/TPP/17-084. PMID: 29309269; PMCID: PMC5760056.
Kraus VB, Blanco FJ, Englund M, Karsdal MA, Lohmander LS. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthritis Cartilage. 2015 Aug;23(8):1233-41. doi: 10.1016/j.joca.2015.03.036. Epub 2015 Apr 9. PMID: 25865392; PMCID: PMC4516635.
Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010 Aug;26(3):355-69. doi: 10.1016/j.cger.2010.03.001. Erratum in: Clin Geriatr Med. 2013 May;29(2):ix. PMID: 20699159; PMCID: PMC2920533.
Osteoarthritis Fact Sheet. World Health Organization.
Understanding Hip Osteoarthritis. Arthritis Foundation.
Katz JN, Arant KR, Loeser RF. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021 Feb 9;325(6):568-578. doi: 10.1001/jama.2020.22171. PMID: 33560326; PMCID: PMC8225295.
Sen R, Hurley JA. Osteoarthritis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482326/
Osteoarthritis of the hip: Aetiology, pathophysiology, and current aspects of management. ResearchGate.
van Berkel AC, Schiphof D, Waarsing JH, Runhaar J, van Ochten JM, Bindels PJE, Bierma-Zeinstra SMA. 10-Year natural course of early hip osteoarthritis in middle-aged persons with hip pain: a CHECK study. Ann Rheum Dis. 2021 Apr;80(4):487-493. doi: 10.1136/annrheumdis-2020-218625. Epub 2021 Jan 15. PMID: 33451999; PMCID: PMC7958083.
Clynes MA, Jameson KA, Edwards MH, Cooper C, Dennison EM. Impact of osteoarthritis on activities of daily living: does joint site matter? Aging Clin Exp Res. 2019 Aug;31(8):1049-1056. doi: 10.1007/s40520-019-01163-0. Epub 2019 Mar 21. PMID: 30903599; PMCID: PMC6661019.
Osteoarthritis of the Hip. Radiopaedia.
Osteoarthritis of the Hip: Clinical Practice Guideline. American Academy of Orthopaedic Surgeons.