Gonarthrosis, also known as knee osteoarthritis or osteoarthritis of the knee, is a common degenerative joint condition that affects millions of people worldwide. It occurs when the protective cartilage in the knee joint gradually wears down, leading to pain, stiffness, reduced mobility, and functional limitations. As one of the most frequent forms of arthritis in the knee, gonarthrosis can significantly impact daily activities and quality of life.
Although gonarthrosis is more common with aging, it can also affect younger individuals due to injury, excessive joint stress, obesity, or biomechanical abnormalities. Understanding the causes, recognizing early symptoms, and choosing effective treatment options are essential for slowing disease progression, reducing pain, and maintaining knee function.
Gonarthrosis Definition: What Is Gonarthrosis of the Knee and Why Does It Develop?
Gonarthrosis, also known as knee osteoarthritis or osteoarthritis of the knee, is a chronic degenerative joint disease that affects the knee joint. It is characterized by the gradual breakdown of articular cartilage, structural changes in the underlying bone, and the development of joint inflammation. These changes lead to pain, stiffness, swelling, and reduced mobility of the knee.
As one of the most common forms of arthritis in the knee, gonarthrosis develops as a result of both natural aging processes and various risk factors. These include excess body weight, previous knee injuries, genetic predisposition, repetitive or excessive joint loading, and certain metabolic or inflammatory diseases, which will be discussed in more detail below.
What Happens Inside the Knee Joint in Gonarthrosis?
The development of gonarthrosis is a complex process involving multiple interconnected mechanisms. To understand it, it is important to know the structure of healthy articular cartilage. Cartilage is composed of:
- Type II collagen, which provides structural strength
- Proteoglycans, which retain water and provide elasticity
- Chondrocytes, the specialized cartilage cells
- Water, which allows shock absorption and smooth joint motion
In a healthy knee joint, these components are in balance—cartilage breakdown and repair occur continuously and evenly.
In knee osteoarthritis, this balance is disrupted. The process usually begins with cartilage damage affecting the smooth surface that allows frictionless movement, absorbs shock, and distributes load evenly across the joint. Cartilage damage is typically caused by a combination of:
- Mechanical factors, such as repetitive loading, joint deformities, or trauma
- Biochemical factors, including inflammatory mediators and enzymes that degrade cartilage components
As the disease progresses, proteoglycan content decreases, water content increases, collagen structure becomes disorganized, and cartilage loses its elasticity and strength.
These changes lead to cartilage fissures and erosions, which may extend down to the underlying bone. Over time, areas of exposed bone develop as cartilage is lost. Without adequate cartilage cushioning, the knee joint becomes less capable of absorbing forces, resulting in increased stress on the subchondral bone.
In response to this increased stress, the bone adapts by becoming denser and harder, and bony outgrowths known as osteophytes begin to form. At the same time, inflammation of the synovial membrane occurs, releasing inflammatory molecules that further accelerate cartilage breakdown and contribute to pain.
This creates a vicious cycle of cartilage degeneration, inflammation, and bone changes, ultimately leading to chronic pain, swelling, stiffness, and progressive loss of knee function.

Primary vs. Secondary Gonarthrosis
Based on the underlying cause, knee osteoarthritis is classified as either primary or secondary.
- Primary gonarthrosis develops without a clearly identifiable cause and is most commonly associated with aging and genetic predisposition. It typically appears gradually over time.
- Secondary gonarthrosis results from a known cause, such as previous knee injuries, obesity, inflammatory joint diseases, metabolic disorders, anatomical deformities of the knee or lower limb, or other medical conditions. Unlike primary osteoarthritis, secondary gonarthrosis can occur at any age and is often linked to a specific event or condition that damages the joint cartilage.
Risk Factors for Knee Osteoarthritis
Risk factors that increase the likelihood of developing osteoarthritis of the knee can be divided into non-modifiable and modifiable factors.
- Non-modifiable factors include age, sex, and genetic predisposition—factors that cannot be changed.
- Modifiable factors include body weight, physical activity patterns, occupational stress on the knee, previous injuries, and lifestyle habits. Addressing these factors through prevention, lifestyle changes, and proper treatment can significantly reduce the risk of disease progression.
In many individuals, multiple risk factors act together. For example, genetic susceptibility may make knee cartilage more vulnerable to damage, while excessive mechanical load—such as obesity or repeated knee injuries—can accelerate the development of gonarthrosis.
| Risk Factor Group | Risk Factors | Explanation |
|---|---|---|
| Non-modifiable factors |
Age Sex Genetic predisposition |
Increasing age significantly raises the risk of gonarthrosis. Women have a higher risk of developing knee osteoarthritis compared to men. Genetic factors may increase susceptibility to degenerative knee joint disease. |
| Modifiable factors |
Excess body weight Trauma or injury Improper knee loading Metabolic syndrome |
Obesity places increased mechanical stress on the knees and raises the risk of knee osteoarthritis. Repeated or severe knee injuries can significantly increase the risk of osteoarthritis. Repetitive activities involving improper knee loading—common in certain occupations or sports, such as prolonged standing, work on hard surfaces, or frequent bending—can accelerate joint degeneration. Metabolic syndrome (obesity, diabetes, dyslipidemia, and hypertension) increases the risk of knee osteoarthritis by promoting chronic inflammation and insulin resistance; elevated levels of harmful blood lipids negatively affect joint health. |
Symptoms of Arthritis in Knees (Gonarthrosis)
The most common symptom that leads patients to seek medical attention is knee pain. The onset of symptoms is usually gradual, developing over several months or even years. Pain and stiffness of the knee typically occur after prolonged sitting, periods of rest, or following increased physical activity. In the early stages of knee osteoarthritis, symptoms often improve with rest, while in advanced stages, pain may persist even at rest.
Many patients report morning stiffness or stiffness after prolonged inactivity. As gonarthrosis progresses, everyday activities become increasingly difficult, including walking, climbing stairs or inclines, and kneeling. Some individuals also notice cracking or grinding sensations in the knee (crepitus) during movement.
In certain patients, so-called inflammatory flare-ups may occur. These episodes are characterized by knee swelling, intensified pain, a sensation of warmth in the joint, and a reduced range of motion.
Because osteoarthritis of the knee is a progressive condition, symptoms tend to worsen over time, leading to increasing limitations in daily activities and a gradual decline in knee function.
How Is Knee Osteoarthritis Diagnosed?
The diagnosis of knee osteoarthritis (gonarthrosis) is based on a combination of characteristic symptoms, physical examination findings, and imaging studies.
The first step is a detailed medical history (anamnesis), during which the physician gathers information about the duration and nature of knee pain, stiffness, movement difficulties, and any previous knee injuries. This is followed by a physical examination, which assesses knee alignment, range of motion, the presence of swelling, tenderness on palpation, and possible cracking or grinding sensations (crepitus) during movement.
To confirm the diagnosis and determine the severity of osteoarthritis of the knee, plain radiography (X-ray) is most commonly used. Typical X-ray findings include:
- narrowing of the joint space,
- formation of bone spurs (osteophytes),
- thickening and increased density of the bone beneath the cartilage (subchondral sclerosis),
- and, in some cases, the presence of subchondral cysts.
It is important that X-ray images are taken in a weight-bearing (standing) position, as this allows for accurate assessment of joint space narrowing and the extent of cartilage damage.
In most cases, additional imaging studies are not required. However, when there is suspicion of other conditions or associated injuries, magnetic resonance imaging (MRI) may be recommended. MRI is particularly useful for evaluating soft tissue structures such as cartilage, menisci, ligaments, and the presence of early or atypical changes.
Stages of Gonarthrosis According to the Kellgren–Lawrence Classification
There are several grading systems used to assess the severity of gonarthrosis, but the Kellgren–Lawrence (K–L) classification is the most widely used in clinical practice and research. This system is based on plain X-ray findings of the knee joint and helps determine the stage and progression of knee osteoarthritis.
Kellgren–Lawrence Grades of Knee Osteoarthritis
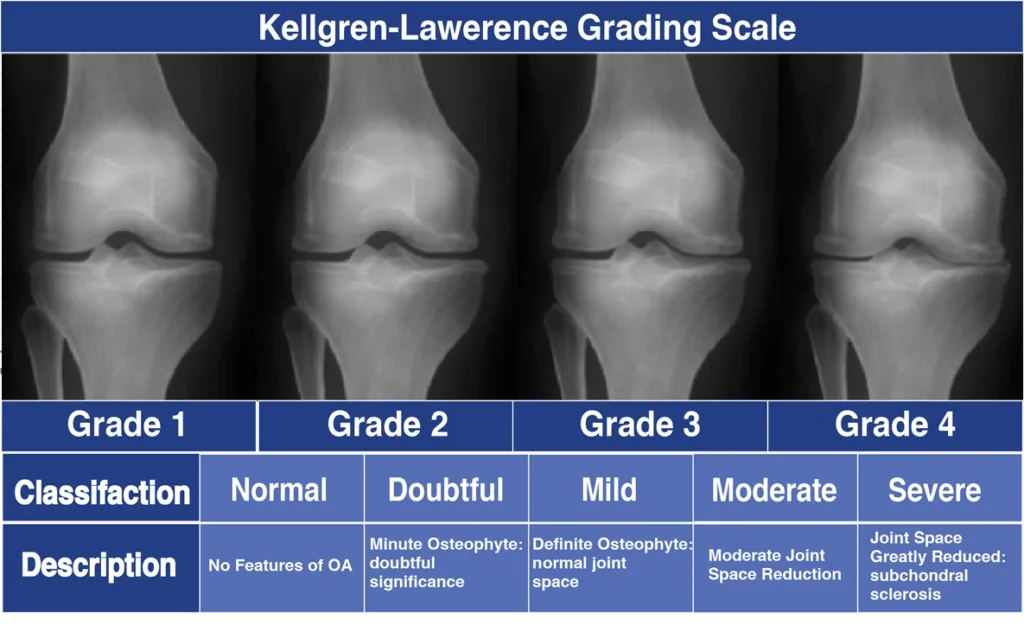
- Grade 0 (None): No radiographic features of osteoarthritisNormal knee joint appearance on X-ray
- Grade 1 (Doubtful): Doubtful or minimal joint space narrowing. Possible early osteophyte formation
- Grade 2 (Mild): Definite presence of osteophytes. Possible narrowing of the joint space
- Grade 3 (Moderate): Multiple moderate-sized osteophytes. Definite joint space narrowing. Evidence of subchondral bone sclerosis. Possible bone contour deformity
- Grade 4 (Severe): Large osteophytes. Marked narrowing of the joint space. Severe subchondral sclerosis. Clear deformity of the joint surfaces
The Kellgren–Lawrence classification is a valuable tool for assessing disease severity, guiding treatment decisions, and monitoring the progression of osteoarthritis of the knee over time. However, it is important to note that radiographic findings do not always correlate perfectly with symptom severity, and clinical evaluation remains essential.
How Gonarthrosis Affects Quality of Life
Knee osteoarthritis (gonarthrosis) can significantly reduce quality of life, especially if it is not recognized and treated early. Pain, stiffness, and reduced mobility make daily activities more difficult, including walking, climbing stairs, rising from a seated position, or performing household tasks. In some patients, pain may even be present at rest or during the night, leading to sleep disturbances and chronic fatigue.
Limited knee function often results in decreased physical activity, which can further contribute to muscle loss, weight gain, and an increased risk of other health problems such as cardiovascular disease and diabetes. Beyond the physical impact, osteoarthritis of the knee can also affect emotional well-being: chronic pain and reduced mobility increase the risk of anxiety and depression.
Gonarthrosis of the Knee – Treatment and Symptom Relief Strategies
Treatment for gonarthrosis of the knee (also known as knee osteoarthritis or osteoarthritis of the knee) is tailored to each patient, depending on the severity of the disease and the symptoms present. In mild to moderate stages, the focus is on pain relief, maintaining mobility, and slowing disease progression through physical therapy, weight management, and anti-inflammatory medications for arthritis in the knee.
For more severe symptoms, or when conservative measures are insufficient, more invasive treatments for knee osteoarthritis may be considered, including joint injections or surgical procedures. Treatment decisions should always be guided by a healthcare professional to ensure maximum effectiveness and preservation of knee function in patients with gonarthrosis.
Below is an overview of the main treatment options for osteoarthritis of the knee.
Treatment options for knee osteoarthritis includes the following key measures:
- Patient education and self-management
- Activity modification and load reduction
- Physical therapy and strengthening exercises
- Weight management and lifestyle adjustments
- Knee braces and orthoses
- Medications (NSAIDs, topical treatments)
- Injections (corticosteroids, hyaluronic acid, PRP)
- Surgical options (arthroscopy, knee replacement)
1. Patient Education
Understanding the nature of knee osteoarthritis, its progressive course, and self-management strategies helps patients make informed treatment decisions and actively participate in their recovery. Proper education can reduce fear of movement and improve independence in daily activities.
2. Activity Modification
Adjusting daily activities to the current state of the knee can significantly reduce joint stress and pain. This includes avoiding repetitive movements that cause discomfort and organizing tasks to balance activity with rest.
Limiting provocative factors—such as prolonged standing, squatting, or carrying heavy loads—helps preserve knee function and reduce the risk of symptom worsening. Small adjustments in routine can have a meaningful long-term impact on quality of life.
3. Physical Therapy and Exercise
Regular exercise under the guidance of a physical therapist, or a tailored home program, can significantly relieve symptoms of gonarthrosis. Exercises improve strength, flexibility, and joint stability, making daily activities easier.
Focus is usually on strengthening the thigh muscles, particularly the quadriceps and hamstrings. Hip muscles—especially the abductors and extensors—should also be strengthened, as they stabilize the knee and reduce joint load.
Physical modalities such as electrotherapy, interferential currents, TENS, and magnetotherapy can help reduce pain. Therapeutic ultrasound or LASER may be beneficial for localized pain, and combining muscle electrostimulation with strength exercises enhances the overall therapeutic effect.
4. Weight Loss
For patients with excess body weight, losing weight can significantly reduce stress on the knee joint, alleviating symptoms and slowing disease progression. This measure is recommended for all stages of knee osteoarthritis in patients with a BMI over 25. A calorie-restricted diet combined with aerobic exercise is the most effective approach.
5. Knee Braces or Orthoses

A knee brace or orthosis is an orthopedic device that helps stabilize the joint, reduce excessive load, and improve mobility. Properly selected braces can reduce pain from the first use and allow patients to stay active despite knee osteoarthritis.
- The level of support depends on the stage of osteoarthritis.
- Valgus (knock-knee) or varus (bow-leg) deformities may require braces with higher support.
- Knee orthoses can redistribute joint load away from the affected compartment, reducing pain and improving function.
Choosing the right knee brace or orthosis can enhance stability, reduce pain, and help patients maintain an active lifestyle despite gonarthrosis.
6. Medications
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help relieve pain and inflammation. Medication choice should always be guided by a physician, considering efficacy, side effects, and medical history.
- Painkillers should be used as needed, rather than continuously, to minimize cardiovascular and gastrointestinal risks.
- Topical anti-inflammatory gels or creams can be applied directly to the knee, reducing systemic exposure while providing local pain relief.
7. Injections
Several types of injections can be administered directly into the knee joint:
- Corticosteroids – used in patients with pronounced inflammation, providing short-term pain relief and reducing swelling.
- Hyaluronic acid (HA) – supplements the joint’s natural lubrication, improving movement and potentially stimulating endogenous HA production.
- Platelet-rich plasma (PRP) – a newer therapy involving injection of concentrated platelets from the patient’s own blood to promote tissue repair and reduce inflammation. Early research shows positive effects on pain reduction and joint function.

8. Surgical Treatment of Gonarthrosis: When Surgery is Needed
Surgery for gonarthrosis or advanced knee osteoarthritis is considered when conservative treatments—such as physical therapy, weight management, medications, or injections—fail to provide sufficient relief. Surgical options depend on the severity of osteoarthritis of the knee, the patient’s age, activity level, and overall health.
- Arthroscopy may be used in selected cases to clean or smooth damaged cartilage in arthritis in the knee.
- Total Knee Arthroplasty (TKA) is often recommended for severe knee osteoarthritis, replacing the damaged joint with a prosthesis to restore function and relieve pain.
Early consultation with an orthopedic specialist ensures that surgery is performed at the optimal time, improving outcomes and maintaining mobility in patients with gonarthrosis. in patients with advanced osteoarthritis, but risks and benefits must be carefully considered.
Prevention and Long-Term Management of Gonarthrosis
Preventing osteoarthritis of the knee progression and managing arthritis in the knee long-term involves a combination of lifestyle modifications and ongoing care:
- Maintain a healthy weight to reduce joint load and slow gonarthrosis progression.
- Engage in regular low-impact exercises, such as swimming or cycling, to strengthen muscles supporting the knee.
- Use appropriate footwear and knee braces when necessary to reduce strain in knee osteoarthritis.
- Monitor symptoms closely and seek early treatment for flare-ups to prevent worsening osteoarthritis of the knee.
Long-term management focuses on preserving joint function, minimizing pain, and supporting a healthy, active lifestyle despite arthritis in the knee.
Final Tips and Key Takeaways
- Early intervention matters: Recognize symptoms of gonarthrosis or knee osteoarthritis early for the best outcomes.
- Conservative management works: Physical therapy, activity modification, weight control, and medications are effective in mild to moderate osteoarthritis of the knee.
- Injections and braces help: Targeted treatments like PRP, hyaluronic acid, and knee orthoses provide relief for arthritis in the knee.
- Surgery is an option: Total Knee Arthroplasty or arthroscopy may be required for severe knee osteoarthritis.
- Lifestyle is key: Maintaining an active lifestyle and healthy weight supports long-term joint health in gonarthrosis.
By understanding and proactively managing osteoarthritis of the knee, patients can reduce pain, maintain mobility, and preserve quality of life.
Thomas S, Browne H, Mobasheri A, Rayman MP. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology (Oxford). 2018 May 1;57(suppl_4):iv61-iv74. PMID: 29684218; PMCID: PMC5905611.
Sophocleous A. The Role of Nutrition in Osteoarthritis Development. Nutrients. 2023 Oct 12;15(20):4336. PMID: 37892417; PMCID: PMC10609695.
Buck AN, Vincent HK, Newman CB, Batsis JA, Abbate LM, Huffman KF, Bodley J, Vos N, Callahan LF, Shultz SP. Evidence-Based Dietary Practices to Improve Osteoarthritis Symptoms: An Umbrella Review. Nutrients. 2023 Jul 6;15(13):3050. PMID: 37447376; PMCID: PMC10347206.
Dairy produce may reduce osteoarthritis risk.
Hsu H, Siwiec RM. Knee Osteoarthritis. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
Berteau JP. Knee Pain from Osteoarthritis: Pathogenesis, Risk Factors, and Recent Evidence on Physical Therapy Interventions. J Clin Med. 2022 Jun 7;11(12):3252. PMID: 35743322; PMCID: PMC9224572.
Primorac D, Molnar V, Rod E, Jeleč Ž, Čukelj F, Matišić V, Vrdoljak T, Hudetz D, Hajsok H, Borić I. Knee Osteoarthritis: A Review of Pathogenesis and State-Of-The-Art Non-Operative Therapeutic Considerations. Genes (Basel). 2020 Jul 26;11(8):854. PMID: 32722615; PMCID: PMC7464436.
Lim WB, Al-Dadah O. Conservative treatment of knee osteoarthritis: A review of the literature. World J Orthop. 2022 Mar 18;13(3):212-229. PMID: 35317254; PMCID: PMC8935331.
InformedHealth.org [Internet]. Osteoarthritis of the knee: Learn More – Joint replacement in osteoarthritis of the knee. [Updated 2024 May 15].
Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016 Aug;474(8):1886-93. PMID: 26872913; PMCID: PMC4925407.