A swollen knee, medically known as knee effusion, occurs when excess synovial fluid builds up in or around the knee joint. This condition can develop for many reasons — ranging from ligament or meniscus injuries to arthritis or inflammation of the bursae, such as prepatellar bursitis.
Along with visible swelling, a knee effusion often causes knee pain, stiffness, and reduced range of motion, making everyday activities like walking, bending, or climbing stairs uncomfortable or even difficult.
In this article, we explain what causes a swollen knee, how knee effusion is diagnosed, and which home treatments and medical options can help relieve symptoms. You’ll also learn when swelling is a warning sign that requires professional medical evaluation.
What Is a Swollen Knee (Knee Effusion)?
The knee is a synovial joint, meaning that the joint surfaces are covered with smooth articular cartilage and enclosed within a strong joint capsule. This capsule is reinforced on the outside by several ligaments, while its inner surface is lined with a thin layer of cells called the synovial membrane.
The primary role of the synovial membrane is to produce synovial fluid, which fills the joint space and allows smooth, pain-free movement. This fluid also nourishes and lubricates the cartilage, helping protect the knee from wear and tear. Under normal conditions, only a small amount of synovial fluid is present inside the joint.
In addition to the joint space, the knee contains several bursae—small, fluid-filled sacs that reduce friction between bones, tendons, and muscles. The most important bursae around the knee include the prepatellar, infrapatellar, and suprapatellar bursae. These structures act as natural cushions, protecting the knee and supporting efficient movement.
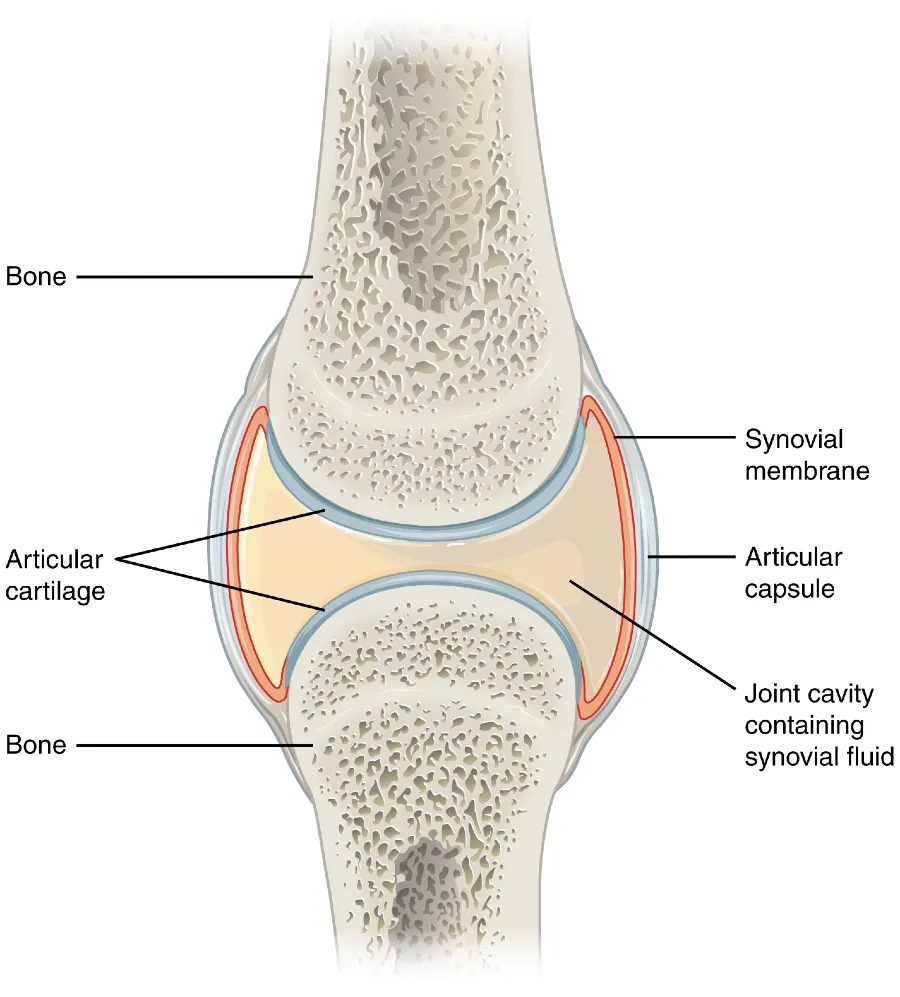
When the knee is affected by injury, overuse, inflammatory conditions, or arthritis, the synovial membrane can become irritated and inflamed. As a result, it thickens and begins to produce excess synovial fluid. When this fluid accumulates within or around the knee joint, it leads to a swollen knee, medically referred to as knee effusion.
What Causes Fluid on the Knee (Knee Effusion)?
A mild knee effusion that does not cause symptoms can sometimes occur in healthy individuals, but a more pronounced swollen knee usually indicates an underlying condition or injury.
Knee effusion can develop for various reasons, including injuries, overuse, or inflammatory and degenerative joint diseases. Common traumatic causes include ligament, bone, and meniscus injuries, as well as overuse syndromes, while non-traumatic causes include knee osteoarthritis, inflammatory arthritis, infections, and crystal deposition disorders such as gout or pseudogout. Tumors are a rare cause of a swollen knee.
In the following sections, we will examine the most common causes of knee effusion in more detail.
1. Knee Injuries
Knee injuries are one of the most common causes of sudden swollen knee and knee effusion. They often occur during sports, falls, or accidents, when a sudden impact, twisting, or overuse damages ligaments, menisci, or the joint capsule. In such cases, the fluid in the knee may be a simple joint effusion, but it can also be blood (hemarthrosis), especially in more severe injuries.
The most frequent acute injuries associated with knee swelling include anterior cruciate ligament (ACL) tears, meniscus injuries, and medial collateral ligament (MCL) sprains. Swelling after an ACL tear usually develops quickly, within a few hours, while meniscus injuries often cause swelling the next day. Patellar dislocation can also lead to sudden knee effusion accompanied by pain and a feeling of instability.
Anyone experiencing significant swelling, severe pain, or a “popping” sensation in the knee should seek prompt evaluation by an orthopedic specialist or trauma physician to determine the exact cause and prevent long-term joint damage.
2. Overuse of the Knee
Simple overuse of a healthy knee rarely causes fluid accumulation. Joint effusion most often occurs when there is pre-existing damage to knee structures, such as the meniscus, anterior cruciate ligament (ACL), or when there is instability, osteoarthritis, or cartilage injury.
In these cases, repetitive stress irritates the synovial membrane, triggering inflammation and excess production of synovial fluid, leading to a knee effusion. These fluid buildups usually develop after intense physical activity—such as hiking, running, or sports—and are accompanied by a feeling of tightness, discomfort, and reduced range of motion, resulting in a swollen knee.
3. Knee Osteoarthritis
Knee osteoarthritis (also called gonarthrosis) is the most common cause of a swollen knee in older adults. This degenerative condition involves gradual breakdown of the cartilage and damage to the joint surfaces and meniscus. In response, the synovial membrane can become inflamed and produce excess synovial fluid, resulting in a knee effusion. Swelling is often accompanied by increased pain, stiffness, and reduced range of motion.
Flare-ups of osteoarthritis and knee effusion typically occur after physical stress on the joint, such as walking, kneeling, or other activities, which further irritate the synovial membrane. The swelling usually lasts from a few days up to several weeks.
4. Inflammatory Rheumatic Diseases
Inflammatory rheumatic diseases, such as rheumatoid arthritis, spondyloarthritis (including psoriatic and reactive arthritis), and Reiter’s syndrome, can lead to a swollen knee. In these conditions, the immune system mistakenly attacks the joint tissues, causing chronic inflammation of the synovial membrane and increased production of fluid, which results in a knee effusion.
The inflammation can also involve surrounding bursae, particularly the suprapatellar and infrapatellar bursae, which may fill with fluid and contribute to additional swelling and discomfort. Unlike injuries, swelling from these conditions often develops spontaneously, may affect multiple joints, and follows a variable course with periods of flare-ups and symptom relief.
5. Joint Infection (Septic Arthritis)
Joint infections, also known as septic arthritis, can cause a sudden and painful swollen knee. Infection usually occurs when bacteria enter the joint—through the bloodstream, after a puncture, surgery, or injury.
The infection triggers intense inflammation of the synovial membrane, leading to the production of large amounts of fluid, often containing pus, resulting in a pronounced knee effusion. Swelling is accompanied by severe pain, redness, and warmth around the joint. General symptoms such as fever, chills, shivering, and fatigue are also common.
Because septic arthritis is a medical emergency that can permanently damage the knee, immediate treatment is required, typically involving joint aspiration, antibiotics, and sometimes surgical drainage.
6. Gout (Crystal-Induced Arthritis)
Gout is an inflammatory joint condition caused by the deposition of uric acid crystals in the joints and surrounding tissues. Although it most commonly affects the big toe, it can also involve the knee, leading to a swollen knee or noticeable knee effusion.
In addition to the joint itself, urate crystals can irritate surrounding structures, including bursae, which may further increase swelling and pain. Gout attacks often come on suddenly and can be extremely painful, requiring prompt medical evaluation and treatment to manage inflammation and prevent joint damage.
7. Knee Bursitis
Bursitis, or inflammation of the bursae around the knee, can be a significant cause of swelling, pain, and limited mobility. Bursae are small, fluid-filled sacs that reduce friction between bones, tendons, and muscles during movement. When a bursa becomes inflamed, its walls thicken, fluid accumulates, and knee effusion develops.
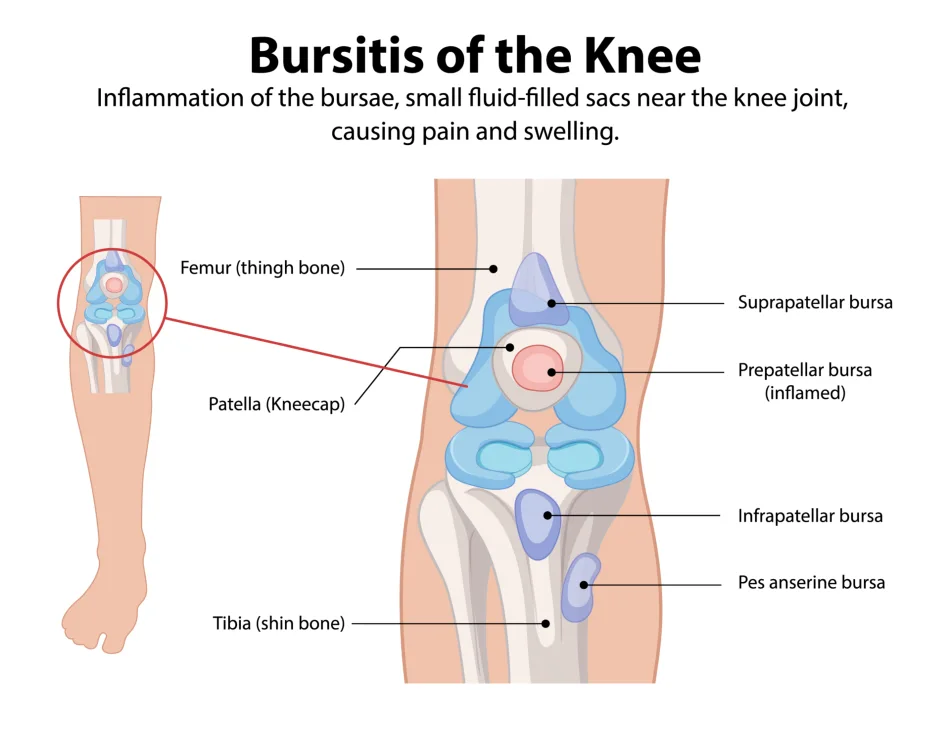
The most commonly affected bursae around the knee include:
- Prepatellar bursa – located just above the patella, between the skin and the kneecap; often inflamed due to frequent kneeling or pressure on the front of the knee (“housemaid’s knee”).
- Pes anserinus bursa – located on the inner side of the knee, a few centimeters below the joint line, where the tendons of three thigh muscles insert on the tibia; inflammation often occurs in overweight individuals or those with slightly misaligned knees.
- Infrapatellar bursa – situated below the patella, between the patellar tendon and the tibia; inflammation can develop due to repeated strain or kneeling (“clergyman’s knee”).

Swollen Knee Symptoms: What to Watch For
The symptoms and signs of a swollen knee depend on the underlying cause of excess synovial fluid. While synovial fluid is essential for joint lubrication, cushioning, and cartilage nutrition, too much fluid often leads to discomfort. Excess fluid in the joint commonly causes pain, swelling, and reduced range of motion, and in cases of inflammatory or infectious causes, warmth and redness may also occur. The most common symptoms are described below:
Swelling
Swelling is the most obvious symptom and can make one knee appear larger than the other. Fluid may accumulate inside the joint capsule or in one of the knee bursae. The degree of swelling can range from mild to pronounced, depending on the cause.
Knee Pain
Pain typically occurs with movement or weight-bearing, while resting may reduce discomfort. The intensity varies—some people experience mild discomfort, while others feel severe pain that limits walking or daily activities.
Stiffness
Excess fluid can make bending or straightening the knee difficult. Stiffness often worsens after periods of rest, such as in the morning or after sitting for a long time.
Muscle Weakness
A swollen knee can inhibit the quadriceps, the main muscle on the front of the thigh. This can lead to rapid loss of strength and muscle mass, affecting walking and joint stability. Patients often notice one thigh appears thinner than the other. This weakness can develop within just a few days of limited knee function.
Reduced Range of Motion
Limited mobility occurs due to pain, swelling, or fluid accumulation. Sometimes, the knee cannot fully bend or straighten.
Warmth and Redness
These symptoms are especially noticeable in inflammatory or infectious causes. The skin over the joint may appear visibly red and feel warmer than surrounding areas.
Inability to Bear Weight
With large effusions or acute injuries, putting weight on the affected knee may be impossible. Intense pain occurs when standing or walking, and sometimes there is a feeling of instability.
Clicking or Locking
Damage to the meniscus or the presence of blood in the joint (hemarthrosis) may cause clicking sounds or occasional “locking” of the knee. These symptoms can make normal movement difficult and require medical evaluation.
Common Symptoms of a Swollen Knee
- Swelling: One knee may appear larger due to excess fluid within the joint or bursae.
- Pain: Usually occurs with movement or weight-bearing, while resting often relieves discomfort.
- Stiffness: Bending or straightening the knee can be difficult, especially after periods of rest.
- Muscle Weakness: The quadriceps may lose strength and bulk, affecting walking and joint stability.
- Reduced Range of Motion: The knee may not fully bend or straighten due to pain or swelling.
- Warmth and Redness: More noticeable with inflammatory or infectious causes; skin may be red and warm to the touch.
- Inability to Bear Weight: Large effusions or acute injuries make standing and walking difficult.
- Clicking or Locking: Can occur with meniscus damage or hemarthrosis, limiting normal movement.
Diagnosis – How the Cause of a Swollen Knee Is Determined
Properly identifying the cause of a knee effusion is crucial for choosing the most effective treatment. Diagnosis typically involves a combination of clinical examination, laboratory tests, and imaging studies.
Clinical Examination
During the examination, the doctor evaluates the joint effusion, pain, warmth, and range of motion of the knee. Specific tests are used to check ligament stability and meniscus function, helping detect any associated injuries that may contribute to the swelling.
Joint Aspiration (Arthrocentesis)
Analyzing the fluid obtained from a joint aspiration can help distinguish different causes of knee effusion. The fluid may be tested for the presence of crystals (as in gout), signs of infection, blood, or inflammatory markers.
Blood Tests
If the swollen knee is red, warm, or particularly painful, the doctor may suspect inflammatory arthritis (such as rheumatoid arthritis, gout, or pseudogout), infection (septic arthritis), or hemarthrosis (blood in the joint). Blood tests are then performed to measure white blood cell count, erythrocyte sedimentation rate (ESR), C-reactive protein, and uric acid levels.
Imaging Studies
Imaging helps confirm the underlying cause and evaluate joint structures:
- X-ray: Useful for detecting degenerative changes but not ideal for assessing fluid accumulation.
- Ultrasound: A non-invasive, readily available method that can quickly detect fluid in the joint or surrounding bursae. It is also valuable for guiding needle placement during aspiration.
- MRI (Magnetic Resonance Imaging): Provides detailed images of ligaments, meniscus, and soft tissues. MRI is recommended in cases of swelling following injury or when the cause remains unclear after physical examination and ultrasound.
What Does Fluid in the Knee Look Like?
Fluid in the knee is actually synovial fluid, a natural joint lubricant that enables smooth movement and nourishes the cartilage. Under normal conditions, synovial fluid is clear, pale yellow (amber-colored), and viscous—often compared to egg white in consistency—which allows it to effectively reduce friction between joint surfaces.
In cases of inflammation, trauma, or infection, the appearance of synovial fluid can change significantly. It may become cloudy, thicker, or less viscous. In bacterial joint infections, the fluid can contain pus and appear yellow-green in color. Cloudy synovial fluid indicates joint irritation, as its composition changes due to the presence of inflammatory cells, proteins, and sometimes microorganisms.
Assessing the appearance of synovial fluid plays an important role in diagnosing the cause of a swollen knee or knee effusion. These visual and laboratory findings help physicians differentiate between traumatic injuries, inflammatory arthritis, infections, and crystal-induced conditions such as gout.

Knee Effusion Treatment
Treatment of a knee effusion depends on the underlying cause of fluid accumulation. Whether the swollen knee develops after trauma, overuse, or as part of osteoarthritis progression, the main goals are to reduce inflammation, relieve symptoms, and prevent further joint irritation.
Home Treatment
Initial management of a swollen knee often starts at home. Rest the affected leg and avoid activities that worsen pain or swelling. Elevating the leg above heart level can help reduce fluid accumulation and promote faster resolution of swelling.
Applying ice wrapped in a towel for 10 to 15 minutes, several times a day, can help decrease inflammation and relieve pain. Cold therapy is particularly useful during the acute phase of knee effusion.
Knee braces or compression sleeves may provide additional support and stability during walking, reducing mechanical stress on the joint. Using a crutch or cane in the opposite hand can further unload the knee and improve comfort while walking. If pain is severe sometimes two crutches are needed.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or ketoprofen, can reduce inflammation and pain and may help decrease swelling. These medications should be used with caution and ideally after consulting a physician or pharmacist, especially in patients with other medical conditions.
How Long Does Knee Effusion Last?
The duration of knee swelling varies depending on the cause. In knee osteoarthritis, knee effusion typically lasts 2 to 3 weeks but may persist for months during periods of disease flare-up.
With mild injuries or overuse, fluid in the knee may resolve within a few days to several weeks, depending on injury severity. In more serious injuries, such as ligament tears—including anterior cruciate ligament (ACL) injuries—swelling can persist for several months.
If the swelling does not improve after 10 to 14 days of conservative treatment, medical evaluation is recommended to identify the underlying cause and adjust treatment accordingly.
Joint Aspiration (Arthrocentesis)
Joint aspiration involves removing excess synovial fluid from the knee using a needle. This procedure often provides immediate relief of pain and swelling. In addition to its therapeutic benefit, the aspirated fluid can be analyzed to determine the cause of the knee effusion.
If fluid reaccumulates, the procedure may be repeated. Arthrocentesis is frequently performed under ultrasound guidance to improve accuracy and safety. During the same procedure, a corticosteroid injection can be administered directly into the knee joint or an inflamed bursa when indicated.
Corticosteroid Injection
Corticosteroid injections into the knee can rapidly reduce inflammation and pain associated with knee effusion. This treatment is particularly effective in inflammatory conditions such as arthritis or bursitis.
The effects usually last several weeks. The number and frequency of injections are carefully considered by the physician to minimize potential side effects and protect joint structures.
Treatment of Inflammatory Conditions
When knee effusion is caused by an underlying inflammatory disease, treatment focuses on controlling the primary condition. Examples include rheumatoid arthritis, gout, pseudogout, and psoriatic arthritis.
Management may involve anti-inflammatory medications, urate-lowering therapy for gout, or immunomodulatory treatments prescribed by a rheumatologist. Adequate control of the underlying disease is essential to prevent recurrent knee effusions and long-term joint damage.
When to See a Doctor for a Swollen Knee (Warning Signs)
Seek medical attention if a swollen knee or knee effusion is accompanied by any of the following:
- Sudden or rapidly increasing swelling, especially after injury
- Severe or worsening knee pain that does not improve with rest
- Redness, warmth, or fever, which may indicate joint infection
- Inability to bear weight or significant knee instability
- Limited range of motion, locking, or catching of the knee
- Persistent swelling lasting longer than 10–14 days despite home treatment
- Recurrent knee effusion that repeatedly returns
- History of recent infection, joint surgery, or immune suppression
- Known inflammatory or rheumatic disease with sudden worsening of symptoms
Prompt evaluation helps identify serious causes such as infection, ligament injury, or inflammatory arthritis and reduces the risk of long-term joint damage.
Conclusion
A swollen knee, also known as knee effusion, can develop for many reasons — ranging from acute injuries and overuse to inflammatory and degenerative joint diseases. Early recognition of the cause and appropriate treatment are essential to preserve knee function, reduce pain, and prevent long-term complications. While home measures may help relieve mild symptoms, persistent, recurrent, or severe swelling should always be evaluated by a medical professional to ensure timely and targeted care.
Frequently Asked Questions
1. How long does a swollen knee last?
The duration of knee effusion depends on the underlying cause. Minor injuries or overuse usually resolve within a few days to two weeks. Swelling from osteoarthritis or inflammatory conditions can persist for several weeks or months. Infections or severe injuries require medical treatment for the swelling to subside.
2. How to reduce swelling in the knee quickly?
To quickly reduce knee swelling, rest the joint, elevate the leg above heart level, apply ice packs for 10–15 minutes several times a day, and use a compression bandage if needed. Over-the-counter anti-inflammatory medications (NSAIDs) can also help. Seek medical advice if swelling persists or is severe.
3. Can knee effusion be prevented?
Complete prevention is not always possible, but the risk can be reduced by:
- Maintaining a healthy body weight
- Strengthening the quadriceps and leg muscles regularly
- Avoiding overuse or trauma to the knee
- Prompt treatment of injuries and inflammatory conditions
4. Will the swelling come back if the underlying cause is not treated?
Yes. If the underlying condition (e.g., arthritis, gout, chronic injury) is not addressed, fluid may accumulate again. Regular monitoring and treatment of the root cause help minimize recurrence.
5. What are the long-term consequences of untreated knee effusion?
Untreated knee effusion and its underlying cause can lead to:
- Damage to cartilage and ligaments
- Reduced mobility and quadriceps weakness
- Increased risk of chronic pain and osteoarthritis
- In case of infection, permanent joint damage
Momodu II, Savaliya V. Septic Arthritis. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: NCBI
Gerena LA, Mabrouk A, DeCastro A. Knee Effusion. [Updated 2024 Feb 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: NCBI
Seidman AJ, Limaiem F. Synovial Fluid Analysis. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: NCBI
American Family Physician – Knee Effusion
Elsaman AM, Radwan AR, Mohammed WI, Ohrndorf S. Low-dose Spironolactone: Treatment for Osteoarthritis-related Knee Effusion. A Prospective Clinical and Sonographic-based Study. J Rheumatol. 2016 Jun;43(6):1114–1120. doi: 10.3899/jrheum.151200. PMID: 27036390. BMJ Article