Hand tingling — that pins-and-needles sensation or hand numbness — can be a sign of something as simple as temporary nerve pressure or as serious as nerve damage.
Most cases are caused by compression or irritation of nerves in the hand or wrist, such as with carpal tunnel syndrome. Other possible causes include diabetes, vitamin deficiencies, or conditions affecting the spine or brain.
In this article, we’ll explore 7 common causes of hand tingling, how to recognize them, and when to seek medical help.
Why Am I Feeling Hand Tingling? Common Causes Explained
Hand tingling is most often caused by nerve-related issues, ranging from localized compression to widespread nerve damage. The two main mechanisms are:
- Nerve compression or irritation — usually due to physical pressure or injury at specific points along the nerve pathway.
- Peripheral neuropathy — damage to multiple nerves, commonly caused by diabetes, alcohol abuse, vitamin deficiencies, or toxins.
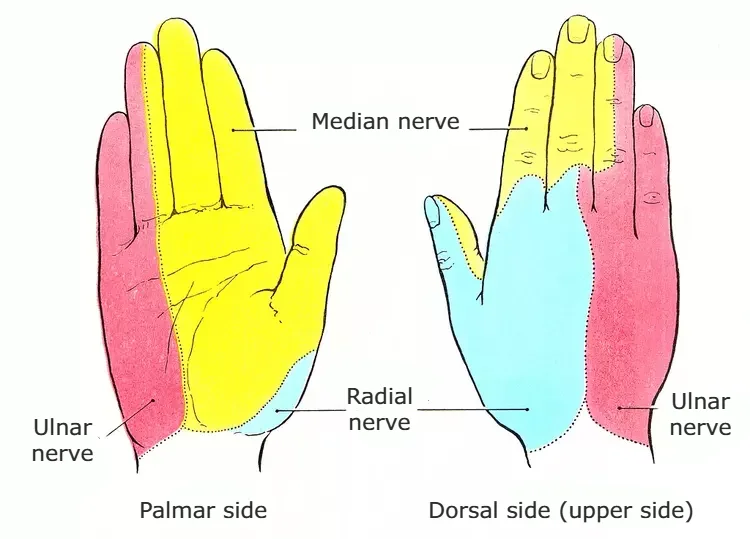
In many cases, nerve entrapment causes tingling in the hands. Nerves that exit the cervical spine travel down the arm through various anatomical tunnels and can be compressed at different locations, including:
- The carpal tunnel (leading to tingling in the thumb, index, and middle fingers — known as carpal tunnel syndrome)
- The cubital tunnel near the elbow (affecting the ring and pinky fingers — cubital tunnel syndrome)
- The cervical spine (due to disc bulging or bone spurs — cervical radiculopathy)
On the other hand, if the tingling is symmetrical and affects both hands and feet in a “glove and stocking” pattern, it may be due to peripheral neuropathy. Common causes include diabetes, chronic alcohol use, age-related nerve degeneration, vitamin B deficiency, and exposure to heavy metals or chemotherapy drugs.
If your symptoms persist, worsen, or affect daily function, it’s important to consult a healthcare professional for proper evaluation and diagnosis.
Hands Tingling: 7 Most Common Causes
In this section, we’ll describe the 7 most common causes of tingling in the hands, how to recognize them, and when to see a doctor.
1. Carpal Tunnel Syndrome
The carpal tunnel is the most common site of nerve compression in the human body. The condition known as carpal tunnel syndrome is a compressive neuropathy caused by compression of the median nerve as it passes through the carpal tunnel in the wrist. It accounts for nearly 90% of all compressive neuropathies. It most often affects people between the ages of 40 and 60, with women being affected ten times more often than men.
In carpal tunnel syndrome, people usually notice symptoms like hand tingling, a prickly or “pins and needles” feeling, and pain. These sensations mostly affect the thumb, index finger, middle finger, and part of the ring finger.In the beginning, symptoms are strongest at night and often wake people up from sleep. They usually try shaking their hands to ease the discomfort. As the nerve damage progresses, other symptoms may appear, such as hand muscle weakness and clumsiness, with patients reporting that objects frequently fall from their hands. In advanced stages, muscle wasting (especially at the base of the thumb) and permanent loss of sensation may occur.
The diagnosis of carpal tunnel syndrome is based on a detailed assessment of symptoms, targeted physical examination, and diagnostic tests. Ultrasound is used to examine the nerve’s structure, and EMG/NCS (electromyography and nerve conduction studies) to assess nerve function.
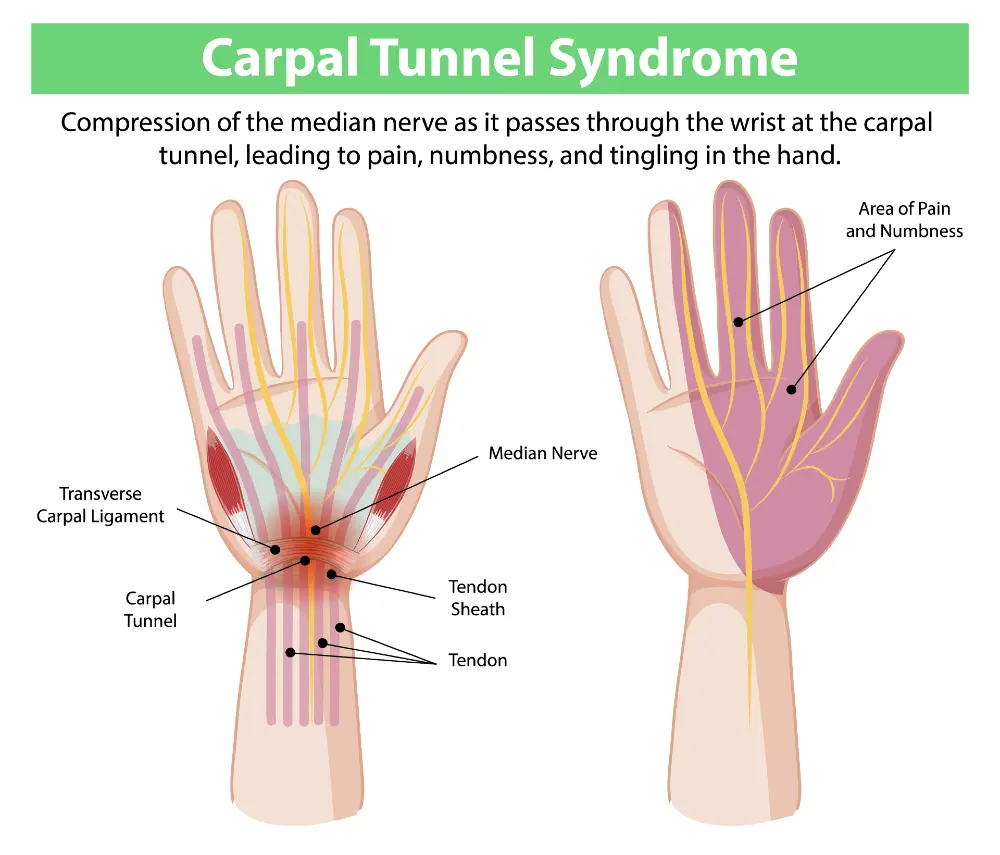
Treatment can be conservative or surgical, depending on the degree of nerve damage and symptoms. Conservative treatment is recommended as the first line of therapy when there is no significant nerve damage. It includes physical therapy, exercises, wearing wrist splints, and corticosteroid injections into the carpal tunnel. Doctors should consider surgical treatment for patients who do not achieve satisfactory improvement or who have advanced nerve damage.
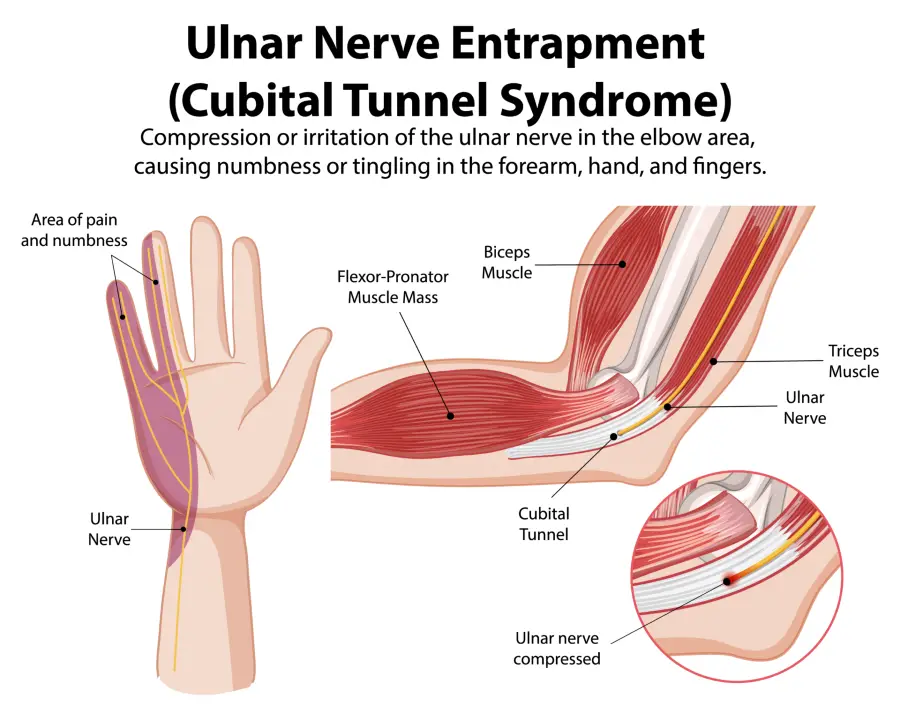
2. Cubital Tunnel Syndrome (Ulnar Nerve Compression at the Elbow)
Cubital tunnel syndrome is the second most common nerve compression problem in the hand. It happens when the ulnar nerve, which runs through a narrow passage called the cubital tunnel at the elbow, gets squeezed or irritated.
The ulnar nerve is one of the three main nerves in the hand and controls some feeling in the palm and fingers, as well as some hand movements.
There are several causes why does cubital tunnel syndrome happens. The most common is putting pressure on the elbow for a long time—like leaning on it a lot or sleeping with your arm bent under your body. Repetitive bending and straightening of the elbow, especially during certain work or activities (like typing or using tools), can also irritate the nerve.
Symptoms
Symptoms usually start slowly and get worse over time, especially if the nerve is strained repeatedly. Common signs include:
- Tingling and numbness in the little finger and ring finger, especially when the elbow is bent.
- Weakness in the hand and fingers, making it harder to hold or grab things.
- Pain around the elbow that can spread down the forearm and into the hand.
- A feeling of weakness and reduced grip strength.
Diagnosis and Treatment
Doctors diagnose cubital tunnel syndrome with physical exams and tests like EMG (electromyography) and ultrasound, which check how well the nerve is working.
Treatment often starts with simple steps like avoiding activities that cause symptoms, wearing a splint to keep the elbow straight at night, and doing physical therapy.
If these methods don’t help or symptoms are severe, surgery might be needed to relieve the pressure on the nerve.
3. Diabetic Polyneuropathy

Diabetic polyneuropathy is one of the most common complications of long-term high blood sugar in people with diabetes. It’s a frequent cause of hand tingling, hand numbness, and pain in the hands and feet.
What is it?
Polyneuropathy means damage to multiple nerves. In diabetes, this happens because high blood sugar levels over time harm the peripheral nerves — the nerves outside the brain and spinal cord.
How Does It Happen?
The main cause is prolonged high blood sugar (hyperglycemia). High sugar levels damage the tiny blood vessels that supply the nerves with oxygen and nutrients. Over time, this lack of support gradually damages the nerves, especially those farthest from the center of the nervous system, such as those in the feet and hands.
Other factors that can speed up nerve damage include high blood pressure, high cholesterol, and smoking.
Symptoms
Symptoms usually appear gradually and begin in the feet, then move upward. Hand symptoms often come later. Common signs include:
- Tingling and numbness in the feet and hands
- Burning or prickling sensations, mainly in the feet
- Numbness and loss of feeling in fingers and palms
- Sharp or stabbing pain, often worse at night
- Muscle weakness in hands or feet
- Reduced ability to feel temperature or touch, which can increase the risk of injuries
The condition usually affects both sides of the body equally and tends to get worse over time.
Diagnosis and Treatment
Doctors diagnose diabetic polyneuropathy based on symptoms, physical exams, and tests like EMG (electromyoneurography). Simple tests can check for loss of sensation using special tools like a monofilament or tuning fork.
Treatment focuses on:
- Controlling blood sugar levels to slow nerve damage and ease symptoms
- Regular doctor check-ups, healthy diet, exercise, and quitting smoking
- Medications to reduce nerve pain, such as certain anti-seizure drugs and antidepressants
- Physical therapy, orthopedic shoe inserts, and sometimes local anesthetics
Early diagnosis and good diabetes control are key to preventing serious problems and managing symptoms better.
4. Cervical Radiculopathy (Neck Nerve Root Irritation)
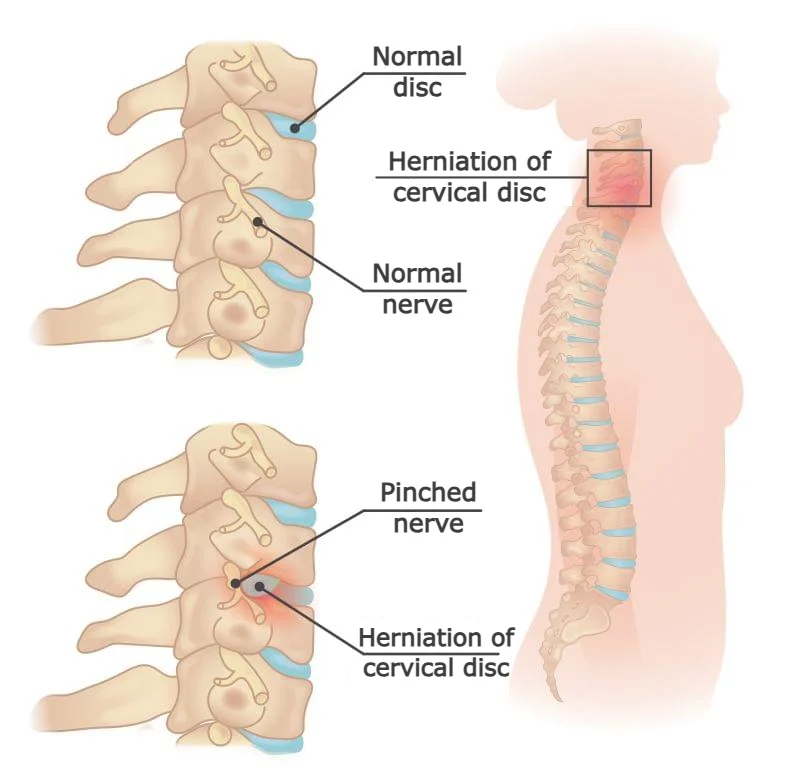
Cervical radiculopathy happens when the nerve roots in your neck get compressed or irritated. These nerve roots come out from the spinal cord in the neck and control feeling and movement in your arms and hands.
What Causes It?
The most common causes are a herniated (slipped) disc, age-related changes like arthritis or bone spurs, and narrowing of the spinal canal (spinal stenosis). These conditions press on the nerves and cause symptoms.
Cervical Radiculopathy Symptoms
- Tingling or numbness in the arms, hands tingling, or tingling in fingers
- Pain that spreads from the neck to the shoulder, upper arm, and hand
- Weakness in arm muscles, trouble with hand movements, and dropping things
- Increased pain or sensitivity when moving your neck
Symptoms can be constant or come and go and often get worse with certain head or neck movements.
Diagnosis and Treatment
Doctors diagnose cervical radiculopathy through physical exams, medical history, and imaging tests like MRI or CT scans. EMG tests can help check nerve damage.
Treatment usually starts with physical therapy, pain relief medicines, and anti-inflammatory drugs. Doctors sometimes use steroid injections to reduce inflammation. If symptoms are severe and don’t improve, surgeons might perform surgery to relieve pressure on the nerves.
Early diagnosis and treatment can help reduce symptoms and prevent further problems.
5. Hand-Arm Vibration Syndrome (HAVS)

HAVS is a health condition caused by long-term exposure to strong vibrations through the hands and arms, usually from using vibrating tools or machines. Over time, these vibrations can damage blood vessels, nerves, muscles, and joints in the hands and arms.
What Causes HAVS?
People who use tools like drills, grinders, saws, hammers, or pneumatic tools a lot are at risk. The constant vibrations cause tiny injuries to the tissues, especially blood vessels and nerves. Workers in construction, mining, metalworking, and forestry are most often affected.
Symptoms
HAVS causes three main types of symptoms:
- Blood vessel problems:
Fingers may turn pale, feel cold, and hurt, especially in cold weather—this is called Raynaud’s phenomenon. - Nerve problems:
Tingling, numbness, and loss of feeling in the hands and fingers. Over time, muscle weakness and difficulty with fine hand movements can occur. - Muscle and joint problems:
Pain, stiffness, and loss of strength in the hands and wrists.
Diagnosis and Treatment
Doctors diagnose HAVS based on your work history, physical exams, and tests that check feeling, blood flow, and hand function. Early diagnosis is important because the condition can cause permanent damage if ignored.
Treatment includes avoiding further exposure to vibrations, wearing protective gloves, and physical therapy to strengthen muscles and improve circulation. Medicines may help improve blood flow or reduce nerve pain.
Prevention
Preventing HAVS means using anti-vibration gloves, taking regular breaks from vibrating tools, and keeping tools well-maintained to reduce vibrations. Employers should educate workers about vibration risks and enforce safety measures.
HAVS is a serious condition that can greatly affect quality of life and the ability to work if not managed properly.
6. Myofascial Pain Syndrome (Neck and Upper Back)
This condition causes pain and tenderness in the muscles and connective tissue (fascia) of the neck and upper back. It often involves “trigger points,” which are sensitive spots in the muscles that can cause pain locally or in other parts of the body.
Causes and Risk Factors
Myofascial pain usually happens due to muscle overuse, injury, stress, poor posture, lack of exercise, or sleeping in uncomfortable positions. It’s common in people who sit for long periods, especially women who work a lot on computers.
Other risk factors include a sedentary lifestyle, bad posture, and emotional stress, which can make muscle tension worse.
What Are Trigger Points?
Trigger points are small tight spots in the muscles that can cause pain where they are or refer pain to other areas. They can also cause sensations like burning, tingling, or numbness in the arms, sometimes mimicking nerve problems.
Diagnosis
Doctors diagnose this condition by examining the muscles and checking for trigger points, pain levels, and movement range.
Treatment
Treatment includes physical therapy with stretching exercises, manual therapy, and techniques to release trigger points like dry needling or local anesthetic injections. Medicines such as anti-inflammatory drugs and muscle relaxants can help. Relaxation techniques are also useful to reduce stress and muscle tension.
7. Thoracic Outlet Syndrome (TOS)
Thoracic Outlet Syndrome is a group of problems caused by compression of nerves or blood vessels in the space between the collarbone and the first rib. The main symptoms are pain in the neck, shoulders, and arms, tingling in the hands, and muscle weakness in the arm.
Causes
TOS can be caused by anatomical abnormalities, injuries, poor posture, repetitive movements, or pressure from muscles. Body features like an extra rib or muscle thickening can also increase the risk of developing this syndrome.
Symptoms
The main symptoms of TOS include pain and tingling in the arms, especially when lifting the arms, muscle weakness, and cold or pale hands due to reduced blood flow.
Treatment
Treatment includes physical therapy to improve posture and stretch muscles, pain relief medications, and in some cases, surgery to relieve pressure on nerves or blood vessels.
Frequently Asked Questions (FAQ)
When Should You See a Doctor If You Have Hand Tingling?
It’s important to know that tingling in the hands is never completely normal. If you only feel it once or twice a month, it’s probably not a big problem. Most likely, you slept in a position that stretched or pressed on a nerve in your arm, which can cause tingling when you wake up.
However, if you experience tingling every day or almost every day, this could be a sign of a more serious issue, and you should see a doctor. While tingling in the hands usually isn’t life-threatening (unlike something like a stroke), it’s important to pay attention to your symptoms so you can find the cause and get the right treatment.
Hand Numbness While Sleeping: Possible Causes
In most medical conditions that cause tingling in the hands, symptoms tend to be worse at night or just before falling asleep. There are several reasons for this:
- Body position: While sleeping, improper body positions can stretch or compress nerves for a long time, making hand tingling worse.
- Reduced circulation: At night, slower blood flow can cause fluid to build up in certain parts of the body, putting extra pressure on the nerves.
- Fewer distractions: During the night, the lack of outside stimuli makes the tingling feel stronger because there’s nothing else to take your attention away from the symptoms.
Foot and Hand Tingling: Common Causes
Unlike tingling that affects only the hands—often caused by nerve compression in the arm—foot and hand tingling at the same time is usually linked to other medical conditions. Causes range from harmless to serious, and some require urgent medical evaluation.
Here are the most common causes:
- Diabetic polyneuropathy: One of the leading causes of tingling in both hands and feet due to long-term high blood sugar damaging peripheral nerves.
- Systemic diseases: These include kidney and liver disorders, blood vessel damage, blood diseases, amyloidosis, connective tissue diseases, chronic inflammation, and hormonal imbalances like hypothyroidism.
- Vitamin deficiencies: Vitamins E, B1, B6, B12, and niacin are crucial for healthy nerve function. A B12 deficiency can lead to pernicious anemia, a known cause of peripheral neuropathy. However, too much B6 can also cause tingling symptoms.
- Alcoholism: Poor nutrition in alcoholics often leads to vitamin deficiencies, especially thiamine. Alcohol itself is also toxic to nerves, increasing the risk of nerve damage.
- Toxins and medications: Exposure to heavy metals (lead, mercury, arsenic, thallium) and certain chemicals, as well as medications used in cancer treatment, antivirals, and antibiotics, can damage nerves.
- Multiple sclerosis (MS): An autoimmune disease that affects the protective covering of nerve fibers in the brain and spinal cord. Tingling in the limbs is a common early symptom.
- Drug use: Certain medications and recreational drugs can trigger tingling in the hands and feet.
- Cervical myelopathy: This condition results from spinal cord compression in the neck, usually due to disc herniation or bone overgrowth. It can cause numbness, weakness, stiffness in the arms and legs, coordination problems, and—in severe cases—bladder or bowel dysfunction. Early diagnosis is essential.
- Anxiety: Anxiety and stress can cause tingling in the hands, feet, face, or around the lips—often due to hyperventilation, which changes blood CO₂ levels. Muscle tension from stress may also compress nerves and worsen tingling sensations.
- Fibromyalgia: A chronic pain condition that increases nerve sensitivity and can cause tingling in hands and feet, along with muscle pain, fatigue, and stiffness.
- Infections: These include Lyme disease, shingles (varicella-zoster), cytomegalovirus, Epstein-Barr virus, herpes simplex, and HIV/AIDS.
- Autoimmune diseases: These include conditions such as CIDP (chronic inflammatory demyelinating polyneuropathy), Guillain-Barré syndrome, lupus, and rheumatoid arthritis.
- Inherited disorders: Some genetic disorders affect the sensory and motor nerves. The most common is Charcot-Marie-Tooth disease.
Pal B. 10-minute consultation: Paraesthesia. BMJ. 2002 Jun 22;324(7352):1501. doi: 10.1136/bmj.324.7352.1501. PMID: 12077040; PMCID: PMC116450.
Sharrak S, Das JM. Hand Nerve Compression Syndromes. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Özdemir G. Working hand syndrome: A new definition of non-classified polyneuropathy condition. Medicine (Baltimore). 2017 Jun;96(25):e7235. doi: 10.1097/MD.0000000000007235. PMID: 28640120; PMCID: PMC5484228.
Mass General: Numbness and Tingling
AAOS: Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome)
Chauhan M, Anand P, Das JM. Cubital Tunnel Syndrome. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Shen SC, House RA. Hand-arm vibration syndrome: What family physicians should know. Can Fam Physician. 2017 Mar;63(3):206-210. PMID: 28292796; PMCID: PMC5349719.
Donnally III CJ, Hanna A, Odom CK. Cervical Myelopathy. [Updated 2023 Jan 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Kaplan J, Kanwal A. Thoracic Outlet Syndrome. [Updated 2023 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Trnci u rukama: 7 najčešćih uzroka i kako ih prepoznati (Fizijatar.hr)
Bodman MA, Dreyer MA, Varacallo M. Diabetic Peripheral Neuropathy. [Updated 2024 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.