Why Does My Heel Ache — it’s a question many people ask when even simple steps become painful. Heel discomfort is surprisingly common and can affect everyone from athletes and outdoor workers to people who spend most of their day sitting. Your heel absorbs the brunt of your body weight with every step, making it especially vulnerable to strain, inflammation, or injury.
In this article, we’ll explore 9 of the most common reasons behind heel ache, how to tell them apart, and what treatments can help. If you’ve been wondering Why Does My Heel Ache, this guide will help you find clarity — and relief.
Heel Anatomy: What’s Inside Your Heel?
The heel is a complex structure that plays a key role in supporting your body and absorbing shock with every step. At its core lies the calcaneus — the heel bone — which is the largest bone in the foot and forms the foundation of the rearfoot.
Attached to the bottom of the heel is the plantar fascia, a thick band of connective tissue that stretches toward the toes and helps maintain the arch of the foot. The Achilles tendon, the body’s strongest tendon, connects the calf muscles to the heel bone. It plays a key role in walking, running, and jumping.
Along the medial (inner) and lateral (outer) sides of the heel pass several important tendons that allow smooth and controlled foot movement:
- Medial side: tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus
- Lateral side: peroneus longus and peroneus brevis tendons
Together, these structures allow the heel to function as both a shock absorber and a lever — but when even one component is irritated or injured, pain can quickly develop.
Who Gets Heel Ache Most Often?
Heel pain can affect people of all ages, but certain groups are more prone to it due to age, activity level, or specific physical factors:
- Older adults: It’s estimated that up to one-third of people over the age of 65 experience some form of heel ache. In this age group, pain is often linked with reduced mobility, balance issues, and a higher risk of falls. Over time, the fatty pad under the heel can thin out (fat pad atrophy), making the heel more vulnerable to impact and strain.
- Physically active individuals over 40: As we age, soft tissues lose elasticity and take longer to recover from stress. Even regular activities like walking or exercise can lead to overuse injuries and heel pain in this group.
- Children and adolescents (ages 8–13): Active kids, especially those involved in sports, may develop heel pain due to a condition called Sever’s disease. The pain usually appears at the back or sides of the heel and is related to growth plate inflammation.
- Athletes of all ages: Sports involving running, jumping, or repetitive loading (like ballet or soccer) place constant stress on the heel and surrounding tissues, increasing the risk of injury.
- People with unilateral heel pain: Pain that starts in one heel can sometimes lead to issues in the opposite heel over time. This usually happens due to altered walking mechanics and overcompensation on the “healthy” side.
What Increases the Risk of Heel Pain?
Regardless of age, certain risk factors significantly increase the likelihood of developing heel pain:
- Foot structure and mechanics – Flat feet, high arches, or excessive pronation during walking
- Tight muscles and poor flexibility – Especially in the calves and hamstrings
- Leg length differences
- Obesity – Extra body weight adds stress to the heel with every step
- Repetitive or physically demanding work – Jobs that involve heavy lifting, jumping, or long periods of standing
- Improper footwear – Unsupportive shoes can lead to uneven pressure and strain
- Pregnancy – Increased weight and fluid retention can contribute to heel discomfort
By identifying these factors early, you can take steps to reduce strain, support your feet properly, and lower your chances of chronic heel pain.
Symptoms of Heel Ache
Heel ache can feel very different depending on the underlying cause. It may come on suddenly or gradually, feel sharp or dull, and occur in different parts of the heel — such as:
- At the back of the heel
- On the inner (medial) side
- On the outer (lateral) side
- Underneath the heel, on the sole of the foot
While each condition has its own unique symptom pattern, there are some common features to look out for.
General symptoms of heel pain may include:
- Tenderness and swelling at the site of pain
- Pain that worsens with pressure, walking, or running
- A burning, stabbing, or throbbing sensation
- Heel pain / Morning stiffness or pain after rest (common in plantar fasciitis)
- Heel pain in the back of the heel, especially with tight shoes (suggestive of Achilles issues)
- Redness or warmth, indicating inflammation
- A bony bump or lump, particularly in cases like Haglund’s deformity
Examples based on pain location:
- Bottom of the heel: Plantar fasciitis often causes sharp pain near the inside edge of the heel, worst with the first steps in the morning or after sitting.
- Back of the heel: Achilles tendinitis usually begins as a dull ache that worsens with activity. You might also notice redness, swelling, or a bump at the tendon attachment point.
- Side of the heel: Pain on the inner or outer side of the heel may be due to nerve compression, tendon strain, or even a stress fracture.
In most cases, a detailed medical history and physical examination can help pinpoint the cause of the pain. Imaging (like X-rays or MRI) may be needed for a confirmed diagnosis.
In the next sections, we’ll look more closely at the most common causes of heel pain based on their location and symptom patterns.
Conditions That Cause Pain Under the Heel
Pain under the heel — often described as a stabbing or bruised sensation — is one of the most common heel complaints. This area is subject to constant impact when walking, running, or standing, which makes it especially vulnerable to overuse and strain-related injuries.
Here are the most frequent conditions that can cause pain beneath the heel:
1. Plantar Fasciitis
Plantar fasciitis is the most common cause of heel pain, particularly in people who are active, overweight, or spend long hours standing. It involves degeneration and irritation of the plantar fascia — a thick band of tissue that runs along the bottom of the foot and supports the arch. Although the term ends in “-itis,” which suggests inflammation, studies show that the condition is mainly degenerative in nature.
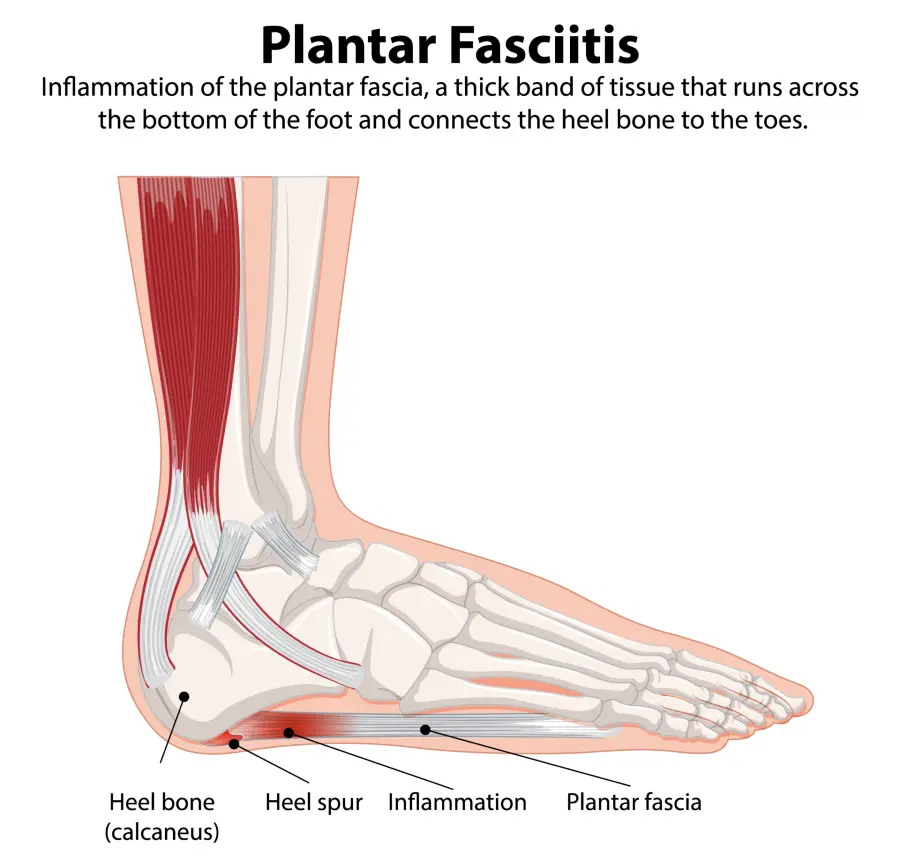
The pain is typically felt on the underside of the heel, slightly toward the inner side, and is often sharp or stabbing. Heel pain is usually worst with the first steps in the morning or after long periods of rest. It may ease with movement but often returns after prolonged activity. Pressing on the affected area often triggers pinpoint pain. A heel spur may also be visible on X-ray, although it doesn’t always cause symptoms.
Most cases improve with conservative treatment, including rest, stretching, ice massage, orthotic insoles, and physical therapy. In more persistent cases, corticosteroid or platelet-rich plasma (PRP) injections may be considered. Night splints and shockwave therapy can also be helpful. Surgery is rarely needed and is reserved for chronic cases that don’t respond to other approaches.
2. Heel Spur (Calcaneal Spur)
A heel spur is a bony outgrowth that forms on place where the plantar fascia attaches to the heel bone. It’s most often associated with prolonged stress on the foot, especially in runners, joggers or individuals with excess body weight. While once thought to result from the plantar fascia pulling on the heel bone, research now suggests that heel spurs form as an adaptive response — helping to distribute load across a wider surface of the heel.
Heel spurs are frequently found incidentally on X-rays, especially in people over 60 and they often coexist with plantar fasciitis. Many people with heel spurs never experience symptoms, while others may develop heel pain due to inflammation of surrounding tissues, nerve compression, or even a stress fracture at the spur site. There’s also a genetic component — some people are simply more prone to forming bony growths, even under normal pressure.

Treatment doesn’t target the spur itself, but rather the underlying condition that’s causing the pain — most commonly plantar fasciitis or heel pad atrophy. Supportive footwear, custom orthotics, stretching, and anti-inflammatory treatments can help relieve discomfort by reducing pressure and irritation in the heel area.
3. Heel Fat Pad Syndrome (Heel Fat Pad Atrophy)
Heel pain caused by fat pad syndrome is usually described as a deep, aching pain in the center of the heel. It can often be triggered by firm pressure to the painful spot — similar to plantar fasciitis — but the underlying cause is different. Instead of inflammation in the plantar fascia, the pain here stems from inflammation, damage, or thinning (atrophy) of the protective fat pad that cushions the heel.
Symptoms tend to worsen when walking barefoot on hard surfaces or during prolonged standing. In some cases, it can be difficult to distinguish fat pad syndrome from plantar fasciitis due to overlapping signs.
Treatment usually involves rest, ice, and anti-inflammatory meds. Heel pads, orthotics, or proper shoes help reduce pressure on the heel.
4. Calcaneal Stress Fracture (Heel Bone Stress Fracture)
A calcaneal stress fracture is a small crack in the heel bone (calcaneus), typically caused by repetitive overuse rather than a single traumatic event. It often develops when healthy bone is subjected to repeated stress without enough time to recover, leading to breakdown and micro-damage. Common triggers include a sudden increase in physical activity, starting a new training routine, weight gain, or wearing improper footwear — especially on hard surfaces.
This injury is frequently seen in runners, military personnel, and athletes involved in high-impact sports. The pain tends to worsen with activity and improve with rest. Symptoms can resemble plantar fasciitis, with tenderness over the heel bone, occasional soft tissue swelling, and rarely, visible bruising. MRI is needed to confirm the diagnosis if an X-ray is inconclusive.
Treatment involves rest from weight-bearing activities for about 6–8 weeks, followed by a structured rehabilitation program to restore strength, mobility, and function in the lower leg.
Heel Pain in the Back: Conditions That Affect the Rear Part of the Heel
Heel pain in the back of the heel is most often linked to problems with the Achilles tendon and surrounding soft tissues. It commonly affects active individuals and those who wear stiff or poorly fitting shoes.
5. Achilles Tendonitis
The Achilles tendon is the strongest tendon in the human body, connecting the calf muscles to the heel bone. It plays a crucial role in walking, running, and jumping. Achilles tendinopathy — often called Achilles tendonitis — is a condition where the tendon becomes painful and thickened due to overuse or degeneration over time. While the term “tendonitis” suggests inflammation, chronic cases usually involve structural changes in the tendon rather than active inflammation.
Achilles tendinopathy is common in runners and people who engage in repetitive or high-impact activities. Other risk factors include aging, poor footwear, lack of warm-up before exercise, being overweight, or training on hard surfaces.
There are two main types:
- insertional (at the point where the tendon attaches to the heel)
- non-insertional (mid-portion of the tendon)
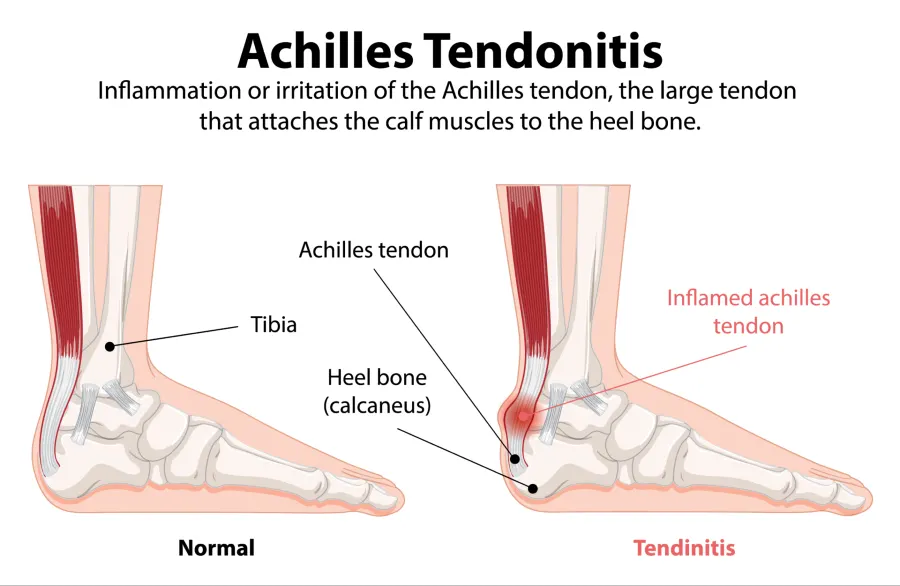
Symptoms often include dull or sharp pain at the back of the heel, stiffness after rest, swelling, and tenderness along the tendon, especially when pressure is applied or during activity.
Treatment is usually conservative and focuses on reducing strain and promoting healing. This includes activity modification, physical therapy, strengthening exercises, proper footwear or orthotic inserts, and anti-inflammatory medications. In persistent or severe cases, more advanced options like injections or surgery may be needed. For a more in-depth guide, see our full article dedicated to Achilles tendon pain and treatment.
6. Haglund’s Disease (Haglund’s Heel)
Haglund’s disease refers to a painful condition caused by a bony enlargement at the upper back part of the heel bone (calcaneus), where the Achilles tendon attaches. This bony prominence — often called a “pump bump” — can irritate the surrounding soft tissues, especially when aggravated by stiff or tight footwear. The exact cause isn’t fully understood, but repetitive pressure and friction on the back of the heel appear to play a major role.
The condition is most common in middle-aged women and often presents as a firm, sometimes red lump on the back of the heel. It typically becomes painful with direct pressure, such as wearing shoes with rigid backs. Haglund’s disease often coexists with Achilles tendinopathy or retrocalcaneal bursitis.
Treatment options include:
- Reducing pressure and inflammation
- Wearing shoes with an open or soft heel area
- Custom orthotic insoles
- Physical therapy
- Anti-inflammatory or pain-relieving medication
- Ultrasound-guided corticosteroid injections
- Surgery in severe or persistent cases to remove the bony prominence
Conditions That Cause Inner and Outer Side Heel Pain
Pain on the inner (medial) or outer (lateral) side of the heel is less common than pain beneath or behind the heel — but it can still signal specific issues. Understanding the exact location of the discomfort is key to identifying the underlying cause.
Pain on the outer or inner side of the heel can be caused by several conditions, but in most cases, the cause is one of the following:
- Outer side heel pain is most often linked to:
- Peroneal tendon tendinopathy or tendinitis
- Sinus tarsi syndrome
- Inner side heel pain is commonly caused by:
- Tarsal tunnel syndrome
- Posterior tibial tendon dysfunction (PTTD)
7. Peroneal Tendonitis
Peroneal tendonitis or peroneal tendinopathy refers to irritation or degeneration of the peronela tendons on the outer side of the ankle and heel — specifically the peroneus brevis and peroneus longus tendons. These tendons stabilize the foot and ankle during walking and running. Overuse or ankle instability can lead to micro-tears, inflammation, and chronic pain.
Symptoms usually include aching or sharp pain behind or below the outer ankle bone, especially during walking, running, or jumping. Pain often improves with rest but returns with activity. In some cases, discomfort may radiate up the outer calf or down to the side of the foot.
Treatment involves reducing load on the tendon during the acute phase (e.g. activity modification, ice, anti-inflammatories), followed by progressive strengthening exercises. Physical therapy, orthotics, and ultrasound-guided injections (e.g., PRP or hyaluronic acid) may also be helpful. Recovery may take weeks to months, depending on severity.
8. Posterior Tibial Tendon Dysfunction
Posterior tibial tendon dysfunction (PTTD) is a condition affecting the tendon on the inner side of the ankle and heel, which plays a key role in supporting the arch and stabilizing the foot. Dysfunction may develop from overuse, trauma, or natural degeneration of the tendon over time.
Symptoms typically include pain and tenderness along the inside of the ankle or heel, which worsens with activity such as walking or standing for long periods. Swelling, foot flattening, or difficulty standing on tiptoe are also common in more advanced stages.
Treatment includes rest, proper footwear or orthotics, strengthening exercises, and physical therapy. In persistent cases, corticosteroid or PRP injections may be considered. Surgery is an option for advanced or non-responsive cases.
9. Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition caused by compression or irritation of the tibial nerve as it passes through the tarsal tunnel, a narrow space on the inner side of the ankle. This tunnel is formed by bone and covered by a strong connective tissue band. Several important structures pass through it, including the tibial nerve, tibial artery and vein, and the tendons of muscles such as the tibialis posterior, flexor digitorum longus, and flexor hallucis longus.
Symptoms often include a sharp, burning pain or tingling and numbness that starts just above the inner ankle and can radiate to the arch of the foot, sole, or even up the calf. The discomfort typically follows the path of the tibial nerve and may worsen with foot dorsiflexion and eversion. Because the symptoms can mimic plantar fasciitis or ankle joint problems, careful clinical evaluation is essential for diagnosis.
Treatment options depend on the severity and underlying cause. Conservative approaches include rest, ice, NSAIDs, and medications for nerve pain (e.g., gabapentin or pregabalin). Physical therapy, nerve gliding exercises, and custom orthotics may help alleviate symptoms and reduce mechanical stress. In cases resistant to conservative treatment, surgical release of the flexor retinaculum may be necessary to relieve pressure on the tibial nerve.
10. Tarsal Sinus Syndrome
Sinus tarsi syndrome refers to pain and discomfort on the outer side of the heel, in the area between the ankle joint and the heel bone. The calcaneus (heel bone) and talus form a joint space called the sinus tarsi. In this condition, inflammation or irritation occurs in the joint capsule and soft tissues within this narrow anatomical channel. It is more commonly seen in dancers, volleyball and basketball players, people with flat feet, excessive foot pronation, and those with excess body weight.
The most common symptom is localized pain in the sinus tarsi area, especially with pressure over the outer ankle or during walking and weight-bearing activities. Many patients also describe a feeling of ankle instability. This sensation often worsens on uneven surfaces or during movements that require quick changes in direction.
Conservative treatment is effective in most cases and includes anti-inflammatory medications, wearing stable footwear, a period of immobilization, and cold therapy. Supportive devices like ankle braces or orthoses can help stabilize the joint. A structured rehabilitation program—focusing on balance, proprioception, and strengthening exercises—is key to full recovery and preventing recurrence.
Frequently Asked Questions (FAQ)
Sever’s Disease and Other Causes of Childhood Heel Pain
Childhood Heel Pain is not uncommon and can stem from several different conditions. The most frequent causes include:
- Sever’s disease (calcaneal apophysitis)
- Achilles tendonitis
- Heel fractures
- Juvenile idiopathic arthritis (JIA)
- Retrocalcaneal bursitis
Among these, Sever’s disease is by far the most common, accounting for up to 90% of heel pain cases in children. It is caused by repetitive stress on the growth plate of the heel bone. The condition most commonly affects physically active children aged 7 to 15, though it can sometimes appear as early as age 5.
A frequent misdiagnosis for pediatric heel pain is plantar fasciitis. While it’s not impossible for children to develop this condition, it is relatively rare in this age group and usually turns out to be Sever’s disease.
The second most common cause of heel pain in kids is Achilles tendonitis. Less common, but still possible, is juvenile idiopathic arthritis (JIA)—a systemic condition that can also affect the heel area.
Because of the unique characteristics of heel pain in children, it’s always best to consult a specialist for an accurate diagnosis and proper treatment.
Heel Pain in the Morning: What’s Causing It?
Waking up with sharp heel pain when you take your first steps out of bed? This is a classic symptom of plantar fasciitis—a condition caused by irritation and microdamage to the plantar fascia, the thick band of tissue connecting your heel bone to your toes. During rest, such as overnight sleep, this tissue tightens. When you stand up, it’s suddenly stretched again, triggering sharp, stabbing pain at the bottom of your heel. The pain often eases with movement but may return after long periods of sitting or inactivity.
Heel Pain Remedy at Home: Simple Ways to Ease Discomfort
Heel pain can make everyday tasks like walking or standing uncomfortable. While medical treatment is sometimes necessary, many people find relief using simple home remedies that reduce inflammation, support healing, and improve foot mechanics.
Stretching and Strengthening Exercises
Gentle stretching of the calf muscles and plantar fascia helps relieve tightness that contributes to heel pain. Try calf stretches against the wall, or roll the sole of your foot over a cold water bottle or massage ball. Toe curls and towel scrunches strengthen the small muscles in your feet and support better alignment.
Supportive Footwear and Insoles
Wearing cushioned, supportive shoes is one of the easiest and most effective ways to reduce heel strain. Orthotic insoles or gel heel cups can redistribute pressure and improve foot posture. Avoid walking barefoot on hard surfaces, especially in the morning.
Cold Therapy and Self-Massage
Applying ice to the heel for 10–15 minutes a few times a day can reduce inflammation and numb pain. Gentle massage around the heel and arch area also helps relax tight tissues and stimulate blood flow.
Maintain a Healthy Body Weight
Excess body weight adds stress to the heel and can worsen pain over time. Even modest weight loss can have a significant positive impact on heel pressure and tissue healing.
Natural Remedies to Try (With Caution)
Some people explore natural options, although evidence is limited. Common choices include:
- Aloe vera gel (applied to soothe irritation)
- Lavender essential oil (mixed with a carrier oil for foot massage or bath soak)
- Ginger root soaks (natural anti-inflammatory properties)
- Willow bark tea (used traditionally for pain relief, drink moderately)
Always test new remedies cautiously, especially with sensitive skin or allergies.
Is Heel Pain a Sign of Cancer?
Heel pain is common — but cancer is not. While it’s understandable to worry when foot pain lingers, most cases of heel pain are caused by benign, treatable conditions. Common culprits include plantar fasciitis, Achilles tendinopathy, heel spurs, and bursitis.
Cancers involving the heel bone are extremely rare. Primary bone tumors such as chondrosarcoma or metastatic lesions can affect the heel, but they usually present with additional warning signs like:
- unexplained weight loss
- night pain that worsens when lying down
- visible swelling or skin changes
- fatigue or systemic symptoms
If your heel pain is persistent, worsening, or comes with unusual symptoms, it’s always wise to consult a healthcare provider. But there’s no reason to panic — serious causes are rare, and early evaluation helps bring clarity and peace of mind.
Remember: Not all persistent pain is dangerous — but all persistent pain deserves attention.
Want to learn more?
If you’re interested in a deeper dive into this topic, be sure to check out our full article:
“Can Heel Pain Be a Sign of Cancer?” — where we explain how to recognize red flags, when to seek help, and how heel pain differs from tumor-related conditions.
Black JR, Hale WE. Prevalence of foot complaints in the elderly. J Am Podiatr Med Assoc. 1987 Jun;77(6):308-11. doi: 10.7547/87507315-77-6-308. PMID: 3612508.
Buchanan BK, Kushner D. Plantar Fasciitis. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2023. PMID: 28613727
Kirkpatrick J, Yassaie O, Mirjalili SA. The plantar calcaneal spur: a review of anatomy, histology, etiology and key associations. J Anat. 2017 Jun;230(6):743-751. doi: 10.1111/joa.12607. Epub 2017 Mar 29. PMID: 28369929; PMCID: PMC5442149.
Italiano J, Bitterman AD. Diagnosis and Management of Calcaneal Stress Fractures. Radiol Technol. 2021 Nov;93(2):177-194. PMID: 34728579.
Weber JM, Vidt LG, Gehl RS, Montgomery T. Calcaneal stress fractures. Clin Podiatr Med Surg. 2005 Jan;22(1):45-54. doi: 10.1016/j.cpm.2004.08.004. PMID: 15555842.
Medina Pabón MA, Naqvi U. Achilles Tendinopathy. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. NCBI
Vaishya R, Agarwal AK, Azizi AT, Vijay V. Haglund’s Syndrome: A Commonly Seen Mysterious Condition. Cureus. 2016 Oct 7;8(10):e820. doi: 10.7759/cureus.820. PMID: 27843738; PMCID: PMC5101401.
Kiel J, Kaiser K. Tarsal Tunnel Syndrome. [Updated 2024 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. NCBI
Sinus tarsi syndrome https://radiopaedia.org/articles/sinus-tarsi-syndrome
Silva GL, Luft C, Lunardelli A, Amaral RH, Melo DA, Donadio MV, Nunes FB, de Azambuja MS, Santana JC, Moraes CM, Mello RO, Cassel E, Pereira MA, de Oliveira JR. Antioxidant, analgesic and anti-inflammatory effects of lavender essential oil. An Acad Bras Cienc. 2015 Aug;87(2 Suppl):1397-408. doi: 10.1590/0001-3765201520150056. Epub 2015 Aug 4. PMID: 26247152.
Bol u peti: 9 glavnih uzroka i kako ih liječiti (Fizijatar.hr)